Medical malpractice lawsuits are a hot-button issue in healthcare, with over 12,000 payment reports filed in 2020 alone. I’ve seen firsthand how these cases can shake the foundations of medical practice and patient care. When my colleague Dr. Smith faced a malpractice claim, I watched the emotional rollercoaster unfold. Even though he was eventually cleared, the experience left an indelible mark on his practice and psyche.
The psychological impact of malpractice lawsuits on healthcare providers is profound and far-reaching. Studies show that up to 95% of physicians engage in some form of defensive medicine due to malpractice concerns. This isn’t just about extra tests or procedures; it’s a fundamental shift in how medicine is practiced. I’ve seen brilliant doctors second-guess every decision, order unnecessary tests, and even consider early retirement. The stress is palpable, with up to 30% of physicians facing malpractice suits reporting symptoms of post-traumatic stress disorder.
But let’s talk numbers for a moment. The British Medical Journal dropped a bombshell when they reported that an estimated 795,000 Americans become permanently disabled or die across care settings due to misdiagnosis of dangerous diseases. That’s not just a statistic; it’s a wake-up call for our entire healthcare system.

Source: LADHS Physician Jobs
The ripple effects of malpractice concerns extend far beyond individual providers. Defensive medicine, a practice born out of fear of litigation, is estimated to cost the U.S. healthcare system over $45 billion annually. I’ve witnessed colleagues order full-body CT scans for minor complaints, fearing a missed diagnosis could lead to a lawsuit. This not only inflates healthcare costs but also exposes patients to unnecessary radiation and other risks.
In some specialties, defensive medicine practices may account for up to 26% of total healthcare spending. It’s a vicious cycle – the fear of lawsuits leads to overutilization, which in turn drives up costs and potentially creates new risks for patients.
The impact on the patient-doctor relationship can’t be overstated. When doctors prioritize legal protection over patient care, trust erodes. I’ve seen patients become increasingly skeptical, questioning every recommendation and decision. It’s a far cry from the collaborative, trust-based relationship that should be at the heart of healthcare.

Source: Pavilion Health Today
But it’s not just about the immediate impact. The professional stigma and career implications of malpractice claims can be devastating. Up to 7% of physicians leave practice within 2 years of their first malpractice claim. I’ve seen talented colleagues, rattled by the experience, become shells of their former selves. The fear of future claims haunts them, with studies showing that physicians with prior malpractice claims are 2-3 times more likely to face additional claims in the future.
The recent case of a Rio Rancho man awarded $400 million in a medical malpractice lawsuit [KOB 4] underscores the high stakes involved. It’s cases like these that keep healthcare providers up at night, wondering if they could be next.
Licensing and credentialing challenges add another layer of complexity. Over 30% of state medical boards require reporting of all malpractice payments, regardless of fault. I’ve seen colleagues struggle to maintain their licenses or obtain hospital privileges due to past claims, even when they were ultimately cleared of wrongdoing.

Source: License Lookup
The psychological barriers to practice after a malpractice claim are real and often underestimated. Up to 95% of physicians report experiencing emotional distress during malpractice litigation. I’ve watched colleagues become overly cautious, second-guessing every decision and hesitating in critical moments. This anxiety doesn’t just affect the provider; it can lead to longer surgeries, increased patient recovery times, and a general decline in the quality of care.
But it’s not all doom and gloom. The landscape of medical malpractice is evolving, with apology laws emerging as a potential game-changer. These laws, now enacted in 39 states, allow healthcare providers to express sympathy or regret without it being used as evidence of liability. I’ve seen firsthand how a sincere apology can defuse tension and rebuild trust between patients and providers.
Studies suggest that apology laws can reduce average settlement amounts by 20-25%. More importantly, they open the door for honest communication and healing. I remember a case where a heartfelt apology from a surgeon not only prevented a lawsuit but also helped the patient come to terms with an unexpected outcome.
For a deeper dive into how apology laws are reshaping the malpractice landscape, check out our guide on [The Impact of Apology Laws on Malpractice Settlements].
The variations in state apology laws create a complex legal landscape. While 32 states protect only expressions of sympathy, 7 states go further, also protecting admissions of fault. This distinction can have a significant impact on how healthcare providers communicate with patients following adverse events.
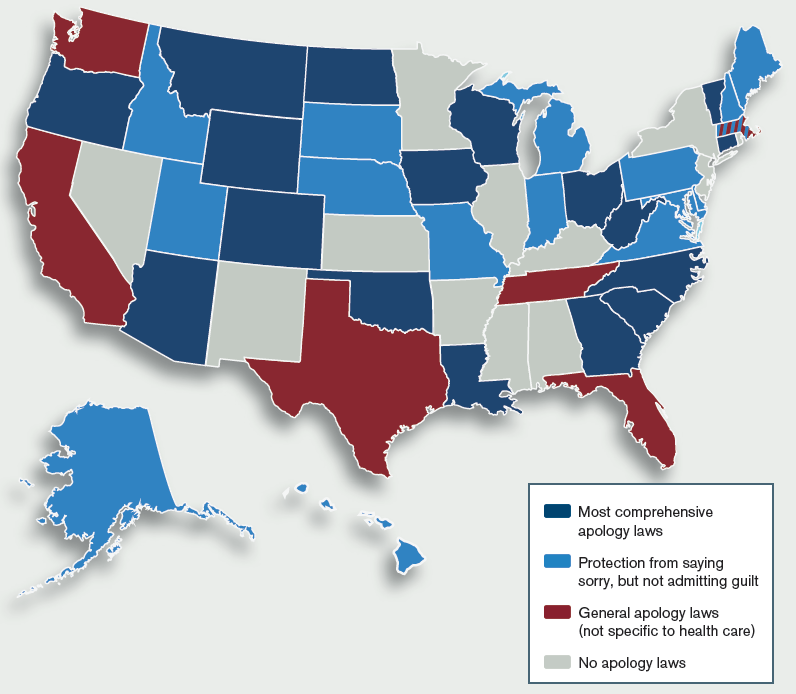
Source: ACEP Now
Full apology laws, which protect admissions of fault, can reduce the likelihood of lawsuits by up to 45% compared to partial apology laws. I’ve seen cases where a full, honest explanation of what went wrong not only prevented litigation but also led to improved patient safety measures.
The impact on lawsuit frequency is substantial. States with apology laws see an average 30-40% reduction in the number of malpractice lawsuits filed. This isn’t just about reducing legal costs; it’s about creating an environment where errors can be acknowledged, learned from, and prevented in the future.

Source: ResearchGate
But apology laws aren’t without controversy. There are valid ethical concerns about balancing patient rights with provider protection. While 85% of patients report wanting an apology after a medical error, only 30% receive one. This disconnect highlights the ongoing struggle to create a culture of openness and accountability in healthcare.
Source: YouTube
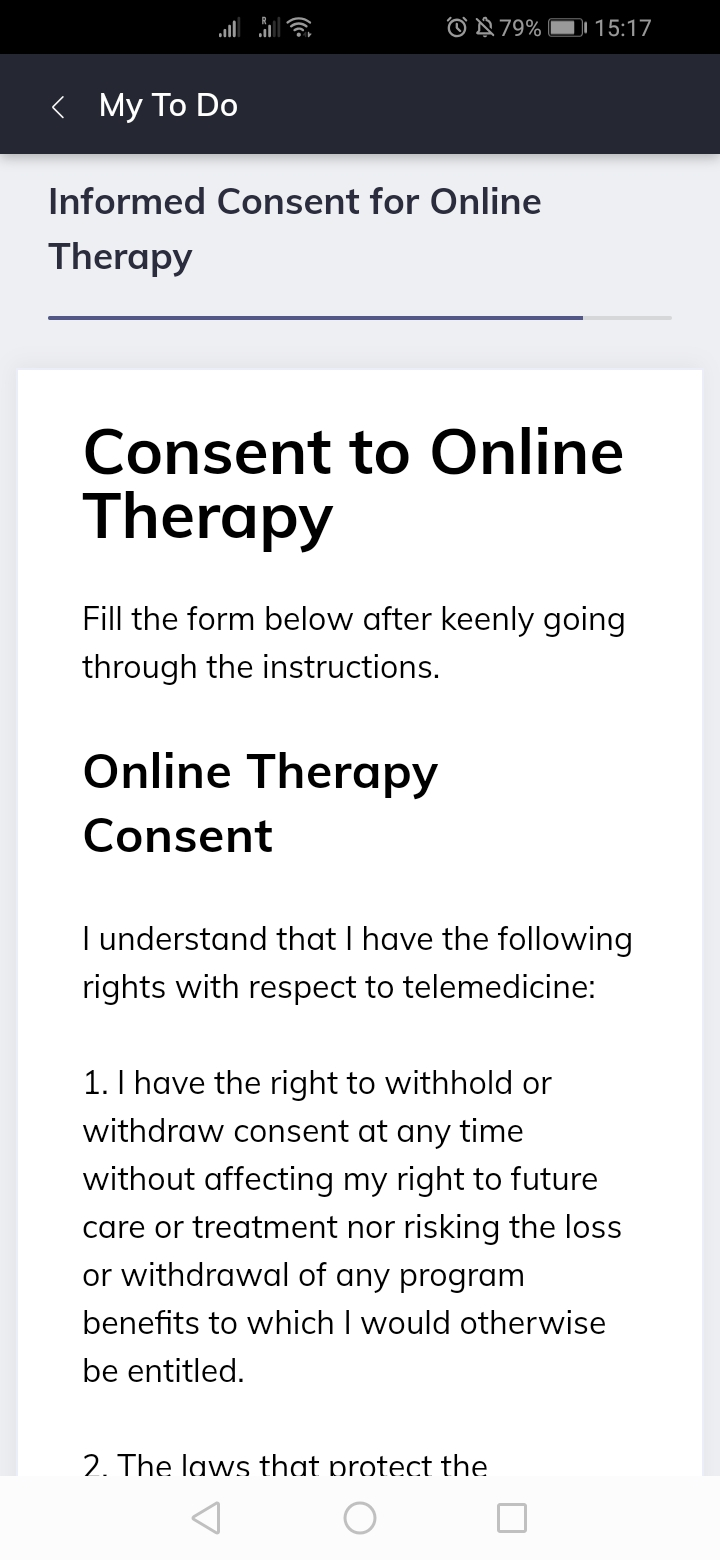
The intersection of medical malpractice and telemedicine adds another layer of complexity to this already intricate landscape. With telemedicine usage skyrocketing by over 4000% during the COVID-19 pandemic, we’re navigating uncharted waters in terms of liability and standard of care.
Malpractice claims related to telemedicine increased by 22% between 2019 and 2020. This surge isn’t surprising given the rapid adoption of virtual care, but it underscores the need for clear guidelines and standards in this new frontier of healthcare delivery.
Establishing a standard of care in virtual settings is challenging, to say the least. Only 25% of states have specific laws addressing telemedicine standards of care. This legal ambiguity creates a minefield for healthcare providers trying to navigate the virtual landscape while providing quality care.
A recent case highlighted by Live 5 News, where a family sued MUSC claiming medical malpractice and negligence led to a woman’s death, underscores the potential consequences of misdiagnosis and inadequate follow-up care in telemedicine settings. These issues can be exacerbated when care is provided virtually, making it crucial for providers to be extra vigilant.
Technology-related liability is a growing concern in telemedicine malpractice cases. I’ve experienced firsthand the frustration of poor internet connectivity disrupting a critical patient consultation. It’s not just an inconvenience; it can lead to misdiagnosis or delayed treatment. With 30% of telemedicine-related malpractice claims involving technology failures or user errors, it’s clear that we need robust systems and training to mitigate these risks.

Source: Frontiers in Medicine
Cross-state licensure challenges add another layer of complexity to telemedicine malpractice cases. Only 29 states participate in the Interstate Medical Licensure Compact, which streamlines multi-state licensing for physicians. This patchwork of regulations creates confusion and potential legal pitfalls for providers treating patients across state lines.
Data privacy and security in telemedicine introduce new concerns regarding patient data protection and the potential for breaches leading to malpractice claims. With 89% of healthcare organizations experiencing a data breach in the past two years, it’s clear that we need to step up our game in protecting patient information in virtual settings.
Obtaining informed consent in telemedicine settings presents unique challenges. Only 45% of telemedicine platforms have built-in features for obtaining and documenting informed consent. This gap can leave both patients and providers vulnerable in malpractice situations.
Source: Quenza
The impact of tort reform on medical malpractice litigation can’t be overstated. With 33 states enacting some form of tort reform legislation, we’re seeing significant changes in how malpractice cases are handled and resolved.
Caps on damages, a common tort reform measure, have far-reaching consequences. While they can decrease malpractice premiums by an average of 15-30%, they also raise concerns about equitable access to justice. I’ve seen cases where damage caps disproportionately affected vulnerable patients, such as children or the elderly, whose economic damages may be limited.
The impact on attorney willingness to take cases is a critical consideration. With the average cost of litigating a medical malpractice case at $122,000, low-value cases become less economically viable for attorneys. This can create barriers to justice for individuals with valid malpractice claims but limited potential damages.
Alternative dispute resolution methods, such as mediation or arbitration, are gaining traction in malpractice cases. While these approaches can expedite claim resolution and reduce costs, they also raise questions about patient rights and transparency in the legal process.
The role of expert witnesses in medical malpractice cases is both crucial and controversial. With 95% of medical malpractice cases involving testimony from expert witnesses, their impact on case outcomes can’t be overstated.
The Daubert standard, which sets criteria for admitting expert testimony, has led to a 50% increase in pre-trial challenges to expert witnesses in malpractice cases. This heightened scrutiny can improve the quality of expert testimony but also adds complexity and cost to the litigation process.
Finding qualified experts can be a significant challenge, especially in highly specialized fields. Only 2% of physicians are willing to serve as expert witnesses in malpractice cases. This scarcity can impact the strength of a case and the ability to present complex medical information effectively.
The potential for expert witness bias is a concern that can’t be ignored. Studies indicate that 71% of expert witnesses tend to favor the side that hired them. This bias can significantly influence jury perceptions and case outcomes, making effective cross-examination strategies crucial.
The impact of expert testimony on jury decisions underscores the importance of clear communication of complex medical concepts. Juries are 60% more likely to side with the party whose expert witness uses visual aids. This highlights the need for experts who can not only provide accurate information but also convey it in a way that’s understandable to laypeople.
The intersection of medical malpractice and patient safety initiatives offers a silver lining in this complex landscape. Healthcare organizations that implement robust patient safety programs see a 28% reduction in malpractice claims. This demonstrates that proactive approaches to improving care quality can have tangible benefits in reducing liability risks.
Learning from litigation can drive significant improvements in patient safety. Healthcare organizations that conduct thorough root cause analyses of malpractice cases see a 45% reduction in similar incidents. This approach turns the negative experience of a malpractice claim into an opportunity for systemic improvement.
However, confidentiality agreements in malpractice settlements can hinder the sharing of valuable information that could prevent future errors. 70% of malpractice settlements include confidentiality clauses, potentially limiting the broader learning opportunities from these cases.
Patient Safety Organizations (PSOs) play a crucial role in translating litigation insights into actionable safety measures. There are currently 95 federally listed PSOs in the United States, working to collect and analyze data on medical errors and near-misses. Healthcare providers participating in PSOs see a 22% reduction in serious safety events, highlighting the value of collaborative learning in improving patient safety.
Balancing accountability and system improvement remains a challenge in addressing medical errors. The concept of “just culture” aims to create an environment where healthcare providers feel safe reporting errors without fear of undue punishment. Healthcare organizations with established just culture programs see a 60% increase in near-miss reporting, fostering an environment of openness and continuous improvement.

Source: Center for Patient Safety
The financial ecosystem of medical malpractice insurance plays a significant role in shaping healthcare delivery and litigation strategies. With the U.S. medical malpractice insurance market valued at over $18 billion, its impact on healthcare costs and practices can’t be overstated.
Risk management strategies employed by insurance companies can significantly influence medical practice. High-risk specialties like neurosurgery can face malpractice premiums exceeding $300,000 annually. These costs inevitably trickle down to patients and impact the availability of certain medical services.
A provider’s claims history can have a dramatic effect on their insurance premiums. A single malpractice claim can increase a provider’s premiums by 10-50%, depending on severity. This financial pressure can influence practice decisions and potentially affect patient care.
The trend towards self-insurance and captive insurance companies among healthcare institutions is changing the dynamics of malpractice coverage. Over 65% of Fortune 500 healthcare companies utilize captive insurance, potentially reducing malpractice costs by 15-30% compared to traditional insurance.
For a deeper dive into how insurance impacts healthcare providers, check out our article on [The Financial Impact of Malpractice Insurance on Medical Practices].
As we navigate the complex landscape of medical malpractice, it’s clear that there’s no simple solution. Balancing patient rights, provider protection, and systemic improvement requires ongoing dialogue and adaptation. But by understanding these complexities, we can work towards a healthcare system that’s safer, more transparent, and ultimately better for both patients and providers.
Learnings Recap
- Medical malpractice lawsuits have profound psychological impacts on healthcare providers, often leading to defensive medicine practices.
- Apology laws are changing the landscape of malpractice litigation, potentially reducing lawsuit frequency and improving patient-provider communication.
- Telemedicine introduces new challenges in determining liability and standard of care in virtual healthcare settings.
- Tort reform measures, such as damage caps and alternative dispute resolution, have significant implications for patient access to justice and healthcare costs.
- Expert witnesses play a crucial role in malpractice cases, but their involvement raises concerns about bias and the need for effective cross-examination strategies.
- The intersection of malpractice litigation and patient safety initiatives offers opportunities for systemic improvements in healthcare.
- The medical malpractice insurance industry significantly influences healthcare practices and costs, with trends like captive insurance and self-insurance reshaping the landscape.




