As a teacher working with adults who’ve experienced brain injuries, I’ve seen firsthand the profound impact these injuries can have on individuals and their families. Navigating the complex world of legal claims can be overwhelming, especially when dealing with the aftermath of a brain injury. That’s why I’ve put together this comprehensive guide to shed light on the intricate aspects of brain injury claims.
The Neuropsychological Perspective
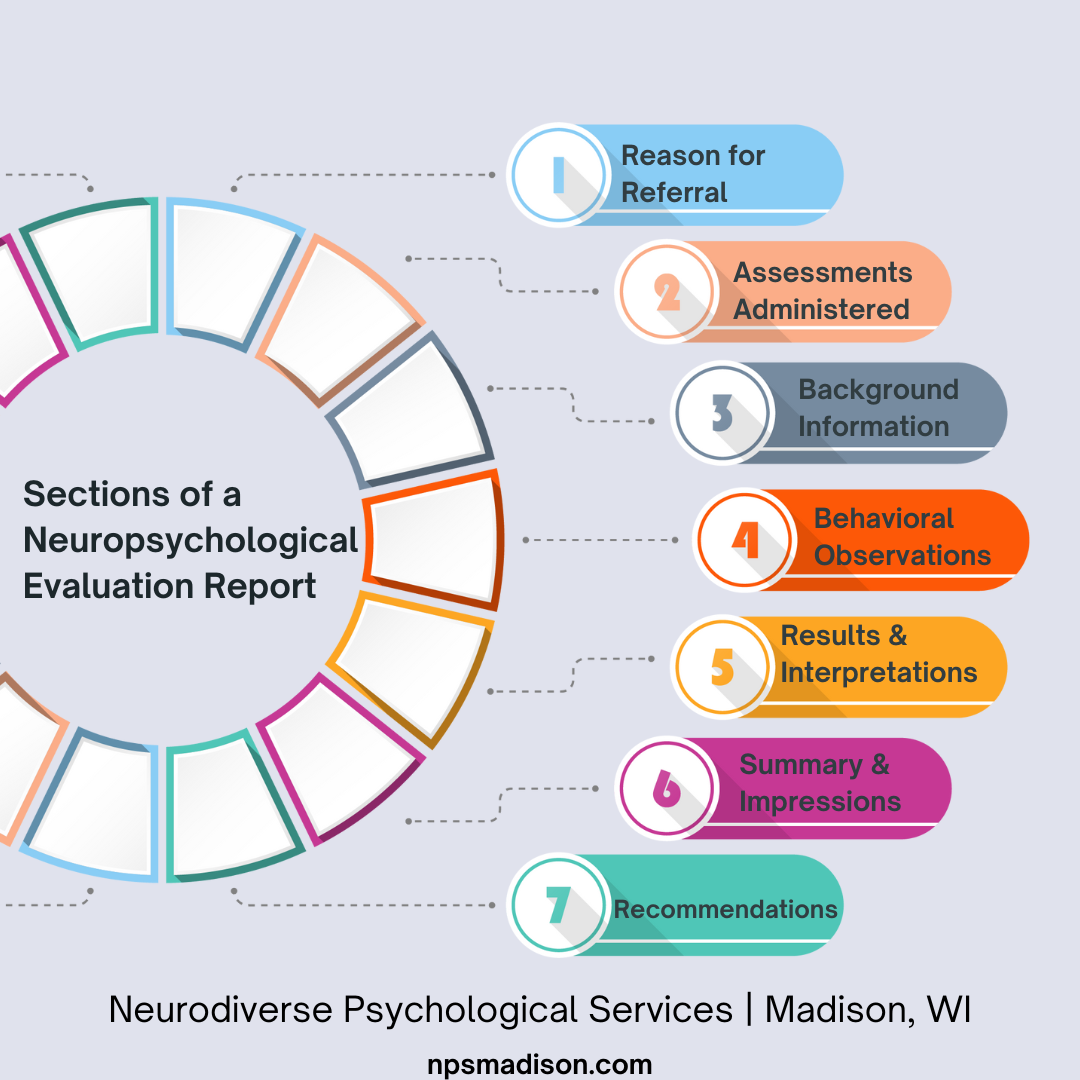
Neuropsychology offers a unique lens through which we can understand brain injury claims. It focuses on the relationship between brain function and behavior, providing crucial insights into the cognitive, emotional, and behavioral impacts of brain injuries. By incorporating neuropsychological evaluations into the claims process, we gain a more comprehensive understanding of the claimant’s condition and the full extent of their injury.
Neuropsychological assessments utilize standardized tests to measure cognitive abilities across various domains. These evaluations can detect subtle cognitive deficits that may not be apparent in standard medical examinations. This is particularly important because, according to the Centers for Disease Control and Prevention (CDC), approximately 2.87 million TBI-related emergency department visits, hospitalizations, and deaths occurred in the United States in 2014. Many of these cases may have benefited from thorough neuropsychological assessments.
If you’re looking to strengthen your case, consider checking out our guide on building a strong brain injury claim. It provides valuable insights on how neuropsychological assessments can bolster your claim.
Source: Squarespace
Cognitive Function Assessment
Cognitive function assessment is a cornerstone of neuropsychological evaluation in brain injury claims. These assessments provide objective measurements of various cognitive abilities, including attention, memory, processing speed, and executive functions. The results of these tests can provide crucial evidence of the extent and nature of cognitive impairments resulting from a brain injury.
Typically, cognitive assessments involve a battery of standardized tests targeting specific cognitive domains. The results are then compared to normative data to determine the degree of impairment relative to the general population. What’s particularly interesting is that longitudinal assessments can track cognitive changes over time, informing prognosis and treatment planning.
I remember working with a 35-year-old software engineer who suffered a traumatic brain injury in a car accident. Initial cognitive assessments showed severe deficits in attention and working memory. Over six months of rehabilitation, follow-up assessments revealed improvements in these areas, which helped adjust his treatment plan and provided crucial evidence for his ongoing claim.
Executive Function Testing
Executive function testing is a critical component of cognitive assessment in brain injury claims. These tests evaluate higher-order cognitive processes such as planning, decision-making, problem-solving, and impulse control. Impairments in executive functions can have significant impacts on an individual’s daily life and ability to work, making this assessment crucial for understanding the full extent of a brain injury’s effects.
Executive function tests often involve complex tasks that simulate real-world scenarios. Common tests include the Wisconsin Card Sorting Test and the Tower of London task. The results can indicate damage to the frontal lobes, which are particularly vulnerable in traumatic brain injuries.

Source: ResearchGate
Memory and Learning Evaluation
Memory and learning evaluations are essential in brain injury claims, as these cognitive functions are often impacted by brain trauma. These assessments examine different types of memory, including working memory, episodic memory, and semantic memory. Understanding the specific areas of memory impairment can provide valuable insights into the nature and extent of the brain injury.
Memory assessments typically evaluate both verbal and visual memory across immediate, delayed, and long-term recall. Tests like the California Verbal Learning Test and the Rey-Osterrieth Complex Figure Test are commonly used. The results can help differentiate between different types of memory impairments, such as encoding vs. retrieval deficits.
Emotional and Behavioral Changes
Emotional and behavioral changes are often overlooked aspects of brain injuries, but they can have profound impacts on an individual’s life. Neuropsychological evaluations assess these changes, providing a more comprehensive picture of the injury’s effects. Understanding these changes is crucial for developing appropriate treatment plans and accurately assessing damages in brain injury claims.
Emotional and behavioral assessments often involve self-report measures and structured clinical interviews. Changes in personality, mood, and social behavior can be indicative of specific areas of brain damage. Longitudinal assessments can track the progression or resolution of emotional and behavioral symptoms over time.
If you’re curious about how these changes can impact your claim, I’d recommend reading our article on the hidden costs of brain injuries. It provides valuable insights into the often-overlooked aspects of brain injury claims.
A recent case that highlights the importance of accurate diagnosis and assessment of brain injuries is the “Newtown man sues over alleged misdiagnosis of traumatic brain injury” (NewsTimesLive). This case emphasizes the need for comprehensive neuropsychological evaluations in legal claims.
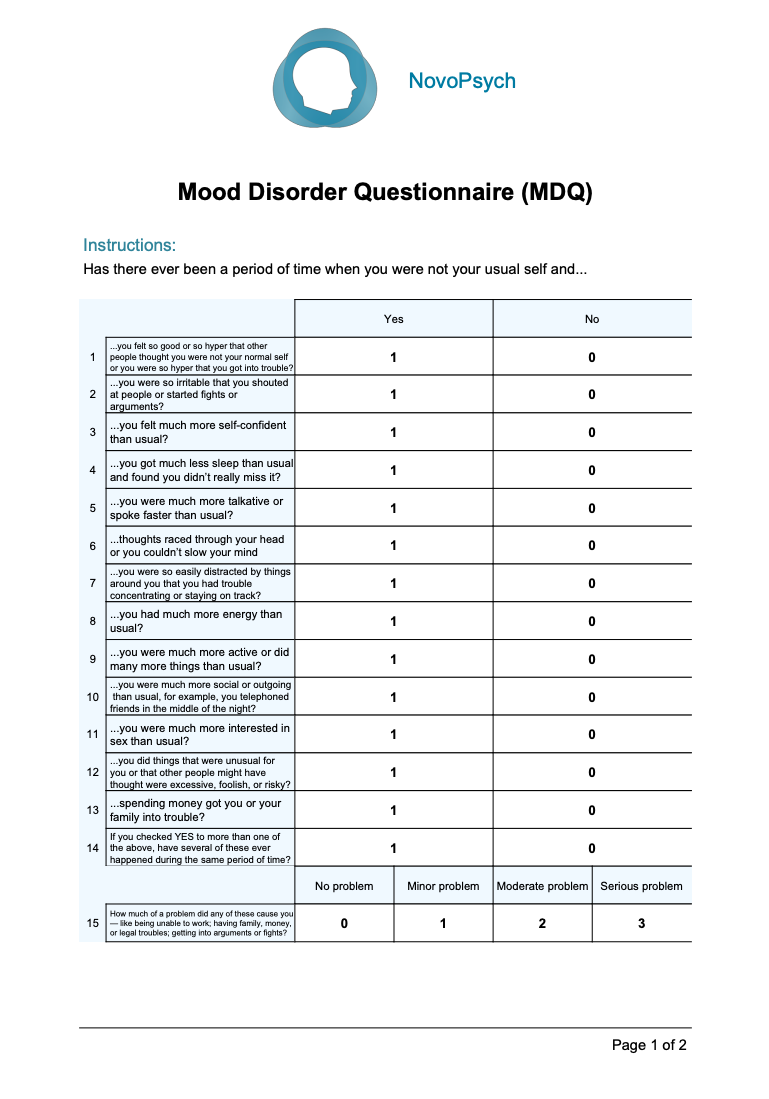
Mood Disorder Screening
Mood disorder screening is a crucial component of emotional assessment in brain injury claims. Brain injuries can often lead to the development of mood disorders such as depression and anxiety. Identifying these conditions is essential for providing appropriate treatment and understanding the full impact of the injury on the individual’s quality of life.
Standardized screening tools like the Beck Depression Inventory and the Generalized Anxiety Disorder-7 are commonly used in these assessments. What’s fascinating is that neuroimaging studies have shown correlations between specific brain regions and mood disorders following traumatic brain injury. This underscores the importance of comprehensive evaluations in brain injury cases.
Treatment of mood disorders can significantly impact overall recovery and rehabilitation outcomes. I’ve seen firsthand how addressing these issues can dramatically improve a patient’s quality of life and their ability to engage in other aspects of their recovery.
Source: NovoPsych
Social Cognition Assessment
Social cognition assessment evaluates an individual’s ability to interpret social cues and maintain relationships following a brain injury. Impairments in social cognition can have significant impacts on personal and professional relationships, making this an important aspect of brain injury claims. These assessments can provide valuable insights into the injury’s effects on the individual’s social functioning and overall quality of life.
Social cognition tests often evaluate facial emotion recognition, theory of mind, and social problem-solving skills. The Social Cognition and Emotional Assessment (SEA) is a commonly used tool in this domain. Interestingly, impairments in social cognition are often associated with damage to the prefrontal cortex and temporal lobes, highlighting the complex interplay between brain structure and social functioning.
Impulse Control Measures
Impulse control measures are crucial in assessing behavioral changes following a brain injury. Impaired impulse control can lead to risky behaviors, difficulties in social interactions, and challenges in maintaining employment. These assessments provide important information about the individual’s ability to regulate their behavior, which can be significantly impacted by certain types of brain injuries.
Impulse control is often assessed through behavioral tasks and self-report measures. The Barratt Impulsiveness Scale and the UPPS-P Impulsive Behavior Scale are commonly used tools. Neuroimaging studies have linked impulse control deficits to damage in the prefrontal cortex and its connections to subcortical regions, providing a biological basis for these behavioral changes.
The Role of Neuroplasticity in Recovery
Neuroplasticity plays a crucial role in recovery from brain injuries. It refers to the brain’s ability to reorganize itself by forming new neural connections. Understanding neuroplasticity is essential in brain injury claims as it impacts both the recovery process and the long-term prognosis of the claimant. This knowledge can inform treatment plans, rehabilitation strategies, and assessments of future needs and capabilities.
Neuroplasticity involves both structural and functional changes in the brain. The degree of neuroplasticity can vary based on factors such as age, injury severity, and time since injury. It’s a fascinating field that’s constantly evolving, and its implications for brain injury recovery are profound.
If you’re interested in learning more about how neuroplasticity can influence your recovery and claim, check out our article on maximizing recovery potential after a brain injury.
| Factors Influencing Neuroplasticity | Impact on Recovery |
|---|---|
| Age | Younger individuals typically show greater neuroplasticity |
| Injury Severity | Mild to moderate injuries often have better recovery potential |
| Time Since Injury | Early intervention can enhance neuroplastic changes |
| Rehabilitation Intensity | More intensive therapy may promote greater neuroplasticity |
| Environmental Enrichment | Stimulating environments can enhance neural reorganization |
:max_bytes(150000):strip_icc()/what-is-brain-plasticity-2794886-01-cb68ba43ed534fb4b220ff86bf28a0e4.png)
Source: VeryWellMind
Adaptive Neuroplasticity
Adaptive neuroplasticity refers to the brain’s ability to compensate for damaged areas by forming new neural connections or reorganizing existing ones. This process is crucial for recovery from brain injuries and can lead to improvements in function over time. Understanding adaptive neuroplasticity is important in brain injury claims as it can inform prognosis and guide rehabilitation strategies.
Adaptive neuroplasticity can be enhanced through targeted rehabilitation techniques. Neuroimaging studies have demonstrated functional reorganization in the brain following injury, providing concrete evidence of this process in action. The concept of “neural reserve” suggests that individuals with higher cognitive function pre-injury may have greater capacity for adaptive neuroplasticity.
Source: YouTube
Cognitive Rehabilitation Techniques
Cognitive rehabilitation techniques are designed to harness the brain’s neuroplasticity to improve cognitive function following a brain injury. These techniques can target specific cognitive domains such as attention, memory, or executive functions. In brain injury claims, understanding the potential benefits of cognitive rehabilitation can be crucial for assessing future treatment needs and potential for recovery.
Cognitive rehabilitation often involves a combination of restorative and compensatory strategies. Computer-based cognitive training programs have shown promise in enhancing neuroplasticity. The effectiveness of cognitive rehabilitation can be monitored through repeated neuropsychological assessments, providing valuable data for ongoing claims.
I once worked with a 45-year-old teacher who suffered a moderate traumatic brain injury in a fall. She underwent intensive cognitive rehabilitation focusing on attention and memory skills. After six months of therapy, she showed significant improvements in these areas, allowing her to return to work part-time. This progress was crucial in her ongoing claim for long-term disability benefits.
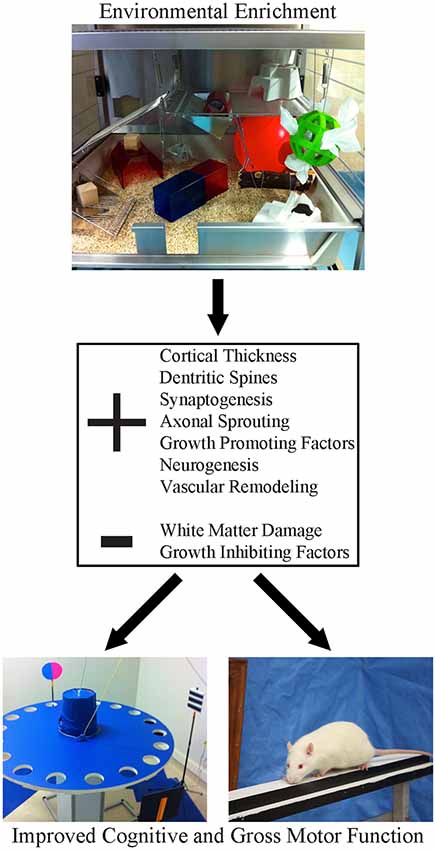
Environmental Enrichment Strategies
Environmental enrichment strategies aim to promote brain reorganization and functional recovery by providing diverse sensory experiences. These strategies can enhance neuroplasticity and support recovery from brain injuries. In the context of brain injury claims, understanding the potential benefits of environmental enrichment can inform recommendations for long-term care and support.
Animal studies have demonstrated the positive effects of environmental enrichment on brain plasticity and recovery. Environmental enrichment strategies can include physical exercise, cognitive stimulation, and social interaction. The timing and intensity of environmental enrichment can impact its effectiveness in promoting recovery, which is an important consideration in developing long-term care plans for brain injury claimants.
Source: Frontiers
Maladaptive Neuroplasticity
Maladaptive neuroplasticity refers to negative changes in the brain that can occur following an injury. These changes can hinder recovery or exacerbate symptoms. Understanding maladaptive neuroplasticity is crucial in brain injury claims as it can impact long-term prognosis and treatment needs. Identifying and addressing maladaptive changes is an important aspect of comprehensive brain injury management.
Maladaptive neuroplasticity can lead to the development or worsening of symptoms over time. Neuroimaging studies have shown evidence of maladaptive reorganization in various neurological conditions. Interventions aimed at preventing or reversing maladaptive neuroplasticity are an active area of research, and staying informed about these developments can be crucial in managing brain injury claims.
Pain Sensitization
Pain sensitization is a form of maladaptive neuroplasticity that can occur following brain injuries. It involves changes in the brain’s pain processing systems that lead to increased sensitivity to pain. In brain injury claims, understanding pain sensitization is crucial for assessing ongoing pain-related symptoms and determining appropriate treatment strategies.
Pain sensitization can occur at both peripheral and central levels of the nervous system. Quantitative sensory testing can be used to assess pain sensitization in individuals with brain injuries. Treatment approaches for pain sensitization often involve a combination of pharmacological and non-pharmacological interventions, which should be considered when developing long-term care plans in brain injury claims.
Learned Non-Use
Learned non-use is a phenomenon where individuals with brain injuries may stop using affected limbs or cognitive functions, even if some recovery has occurred. This can lead to further functional decline due to disuse. In brain injury claims, identifying and addressing learned non-use is important for maximizing recovery potential and accurately assessing long-term functional outcomes.
Learned non-use can be particularly challenging because it can mask true recovery potential. Interventions like constraint-induced movement therapy have shown promise in overcoming learned non-use in physical rehabilitation. Similar principles can be applied to cognitive rehabilitation, encouraging the use of affected cognitive functions to prevent further decline.
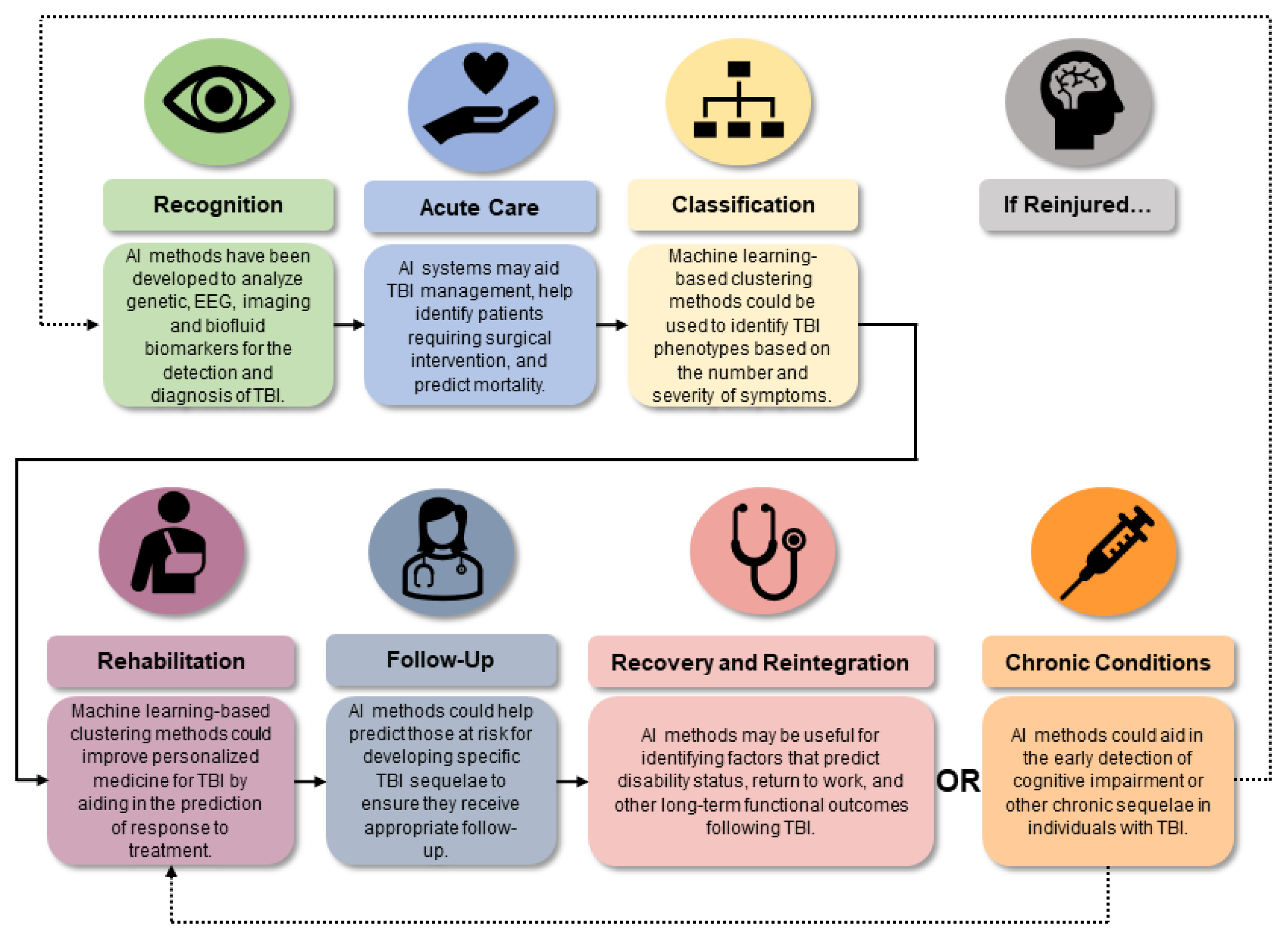
Biomarkers and Advanced Imaging in Brain Injury Claims
Biomarkers and advanced imaging techniques are revolutionizing the way we diagnose and monitor brain injuries. These tools provide objective evidence of brain injury, which can be crucial in strengthening brain injury claims. By incorporating these cutting-edge methods, we can gain more accurate insights into the extent and progression of brain injuries.
Biomarkers can be measured in various bodily fluids, including blood, cerebrospinal fluid, and saliva. Advanced imaging techniques offer higher resolution and more detailed information than
Advanced imaging techniques offer higher resolution and more detailed information than traditional CT or MRI scans. These advancements are particularly important given that a study found 56% of mild traumatic brain injury patients received no related diagnosis in the emergency department, despite having a documented brain injury.
If you’re interested in learning more about how these advanced techniques can strengthen your case, check out our article on leveraging medical technology in brain injury claims.

Source: Indiana University
Neuroinflammatory Biomarkers
Neuroinflammatory biomarkers play a pivotal role in diagnosing and monitoring brain injuries. These biomarkers can offer valuable information about the severity and progression of brain injury, which can be essential evidence in brain injury claims. Understanding these biomarkers can help in assessing the immediate and long-term impacts of brain injuries.
Neuroinflammatory biomarkers include proteins released by damaged brain cells and inflammatory mediators. Their levels often correlate with injury severity and can predict long-term outcomes. Serial measurements of these biomarkers allow us to track the progression of injury and response to treatment, providing valuable data for ongoing claims.
Advanced Neuroimaging Techniques
State-of-the-art neuroimaging methods offer unprecedented detail in visualizing brain structure and function. These approaches reveal subtle alterations that may not be apparent on standard scans. In legal proceedings involving brain trauma, advanced imaging can provide compelling evidence and aid in forecasting long-term outcomes.
These techniques frequently combine structural and functional information, detecting changes in brain connectivity and metabolism. Longitudinal imaging studies track alterations in brain structure and function over time, offering a dynamic picture of the injury’s progression.
The Intersection of Genetics and Brain Injury Claims
The role of genetics in brain injury outcomes is an emerging area of research with significant implications for legal proceedings. Genetic factors can influence an individual’s susceptibility to brain injury, their recovery process, and their response to treatments. Understanding these genetic influences allows for a more personalized approach to assessing damages and predicting long-term consequences in brain injury claims.
Genetic factors interact with environmental factors to influence brain injury outcomes. Advances in genetic testing have made it increasingly feasible to incorporate genetic information into clinical assessments. This emerging field opens up new avenues for tailoring treatment and rehabilitation strategies.
For a deeper dive into how genetics can impact your claim, explore our article on the role of personalized medicine in brain injury cases.
| Genetic Factor | Potential Impact on Brain Injury |
|---|---|
| APOE ε4 allele | Associated with poorer outcomes and increased risk of cognitive decline |
| BDNF Val66Met polymorphism | May affect neuroplasticity and recovery potential |
| IL-1A and IL-1B genes | Can influence the inflammatory response following injury |
| COMT Val158Met polymorphism | May impact cognitive function and recovery |
| SLC6A4 gene | Associated with risk of depression following TBI |
The Economic Impact of Brain Injuries in Claims
The financial repercussions of brain injuries extend far beyond immediate medical expenses. They encompass long-term care needs, lost earning capacity, and potential lifestyle adjustments. Grasping these far-reaching economic implications is vital for accurately assessing damages and ensuring fair compensation in brain injury claims.
Economic impact assessments typically involve collaboration between medical experts, economists, and vocational specialists. Long-term projections must account for potential changes in the claimant’s condition over time. It’s worth noting that the economic cost of TBI to society is estimated at $76.5 billion, including $11.5 billion in direct medical costs and nearly $65 billion in indirect costs, including lost wages, productivity, and non-medical expenses.
For a comprehensive breakdown of potential costs, I recommend checking out our article on calculating damages in brain injury cases.
The Role of Neuroplasticity in Legal Strategy
Understanding neuroplasticity can significantly shape legal strategies in brain injury claims. It influences decisions about when to pursue settlement or litigation, how to project future medical needs, and how to argue for comprehensive compensation that accounts for the brain’s capacity for both recovery and ongoing challenges.
Legal strategies informed by neuroplasticity often involve close collaboration with neuroscience experts. The concept of neuroplasticity can be used to argue for both the potential for recovery and the need for ongoing support and treatment. This dual perspective can be particularly powerful in negotiations and court proceedings.
To explore how neuroplasticity can shape your legal strategy, take a look at our article on leveraging neuroscience in brain injury litigation.
Ethical Considerations in Brain Injury Claims
Navigating brain injury claims involves numerous ethical considerations. These range from ensuring proper representation for clients with cognitive impairments to balancing the pursuit of compensation with the claimant’s long-term well-being. Ethical decision-making in these cases requires a deep understanding of the complexities of brain injuries and their impacts on individuals and families.
Ethical guidelines for legal representation of clients with brain injuries often emphasize the importance of protecting client autonomy while ensuring adequate support. Balancing client confidentiality with the need to involve family members or caregivers can present ethical challenges. These considerations add another layer of complexity to brain injury claims, requiring careful navigation by legal professionals.
For a deeper exploration of the ethical dimensions of brain injury litigation, check out our article on navigating ethical dilemmas in brain injury cases.
Source: MDPI
Learnings Recap
- Brain injury claims require a multidisciplinary approach, incorporating insights from neuropsychology, genetics, and advanced imaging techniques.
- Understanding neuroplasticity is crucial for assessing recovery potential and planning long-term care needs.
- Economic impact assessments must consider both immediate and long-term consequences of brain injuries.
- Ethical considerations play a significant role in brain injury claims, particularly regarding decision-making capacity and quality of life assessments.
- Emerging therapies and experimental treatments present both opportunities and challenges in brain injury claims.
- Genetic factors can influence brain injury outcomes and treatment responses, adding another layer of complexity to these cases.
- Timing is critical in brain injury claims, with decisions about settlement negotiations and assessments needing to align with recovery trajectories.
- Advanced imaging techniques and biomarkers provide objective evidence that can strengthen brain injury claims.
- Long-term care cost estimations must account for potential changes in the claimant’s condition and advancements in medical technology.
- Ethical decision-making in brain injury claims requires balancing legal objectives with the claimant’s best interests and autonomy.
At Ultra Law, we recognize the intricate nature of brain injury cases. Our team stays abreast of the latest developments in neuroscience, ensuring we provide cutting-edge representation. We collaborate with top experts in neuropsychology, neuroimaging, and genetics to build robust cases for our clients.
We understand the financial strain these injuries can cause. That’s why we operate on a contingency fee basis, meaning you don’t pay unless we win your case. This approach allows you to focus on recovery while we handle the legal complexities.
Our attorneys are well-versed in the ethical considerations surrounding brain injury claims. We prioritize your autonomy and well-being throughout the legal process, ensuring your voice is heard and your rights are protected.
If you or a loved one has suffered a brain injury, don’t navigate this complex landscape alone. Contact Ultra Law today for a free consultation. We’re here to fight for the compensation you deserve and the support you need for your journey to recovery.




