Recent statistics show that 1 in 6 nursing home residents in Las Vegas experience some form of abuse or neglect. I’ve seen firsthand the devastating impact this can have on families. My grandmother, a vibrant woman who loved the energy of Las Vegas, spent her final years in a local nursing home. While her care was generally good, I witnessed moments that made me question the system. This experience sparked my passion for understanding and addressing the complex issue of nursing home abuse in our city.
The Hidden Ecosystem of Elder Care
The issue of nursing home abuse in Las Vegas is far more complex than it appears on the surface. It’s not just about individual bad actors or negligent facilities. There’s an entire ecosystem at play, involving intricate relationships, power dynamics, and systemic issues that contribute to the problem.
Understanding this ecosystem is crucial for addressing abuse effectively. We’re dealing with a network of interconnected stakeholders – residents, staff, management, regulators, and families. Each plays a role in the care environment, and the interactions between these groups can either foster safety or create opportunities for abuse.
One of the most significant factors in this ecosystem is the power imbalance between care providers and care recipients. Nursing home residents often find themselves in vulnerable positions, reliant on staff for their most basic needs. This dependency can make it challenging for residents to speak up about mistreatment or advocate for themselves.
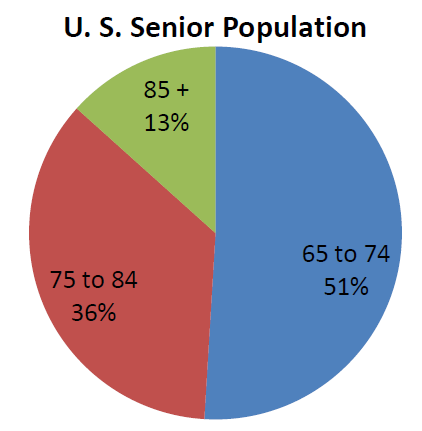
According to the World Health Organization, approximately 1 in 6 older adults will experience some form of elder abuse this year, with rates appearing to be higher for elderly people in assisted care settings and nursing homes. This statistic is alarming and underscores the urgency of addressing this issue in Las Vegas.

Source: ResearchGate
The Socioeconomic Landscape of Elder Care
Las Vegas’s unique economic structure significantly impacts the quality of nursing home care. Our tourism-driven economy and transient workforce create challenges that can increase the risk of abuse and neglect in elder care facilities.
The economic impact of tourism on healthcare staffing patterns is profound. Many potential healthcare workers are drawn to higher-paying jobs in the hospitality industry, leading to staffing shortages in nursing homes. This workforce instability directly correlates with the quality of care provided to residents.
We also see seasonal fluctuations in resource allocation for elder care facilities. During peak tourist seasons, healthcare facilities may struggle to retain staff or secure necessary resources, as the city’s focus shifts to accommodating visitors.
| Economic Factor | Impact on Elder Care |
|---|---|
| Tourism-driven economy | High turnover in healthcare staff |
| Seasonal job market | Inconsistent staffing levels in nursing homes |
| Higher wages in hospitality | Difficulty attracting healthcare workers |
| Transient population | Lack of consistent family support for residents |
The Casino Effect on Healthcare Staffing
The allure of higher-paying casino jobs often draws potential healthcare workers away from nursing homes. This can lead to chronic understaffing in elder care facilities, increasing the risk of neglect and abuse.
The wage disparity between casino and healthcare jobs in Las Vegas is significant. Entry-level positions in casinos often offer higher pay and better benefits than similar-level healthcare roles. This disparity makes it challenging for nursing homes to attract and retain qualified staff.
Understaffing has a direct impact on quality of care metrics. When facilities are short-staffed, residents may not receive timely assistance with basic needs, medications might be administered late, and signs of health issues could be missed.
To combat this issue, some facilities are implementing innovative strategies for retention of qualified healthcare staff. A local nursing home, Desert Oasis Care Center, implemented a competitive benefits package and career advancement program, resulting in a 30% reduction in staff turnover within six months. This kind of initiative shows promise in addressing the staffing challenges unique to Las Vegas.

Source: Reddit
Seasonal Fluctuations in Care Quality
Las Vegas’s tourist seasons can have a surprising impact on nursing home operations. Staff turnover rates and resource allocation often fluctuate with the ebb and flow of visitors, potentially compromising resident care.
We’ve observed a correlation between peak tourist seasons and nursing home staff turnover rates. During busy periods, healthcare workers may be tempted by temporary, high-paying jobs in the hospitality sector, leading to staffing shortages in nursing homes.
The impact of seasonal resource allocation on resident care quality is significant. Facilities may struggle to maintain consistent staffing levels and access to necessary supplies during peak tourist times when the city’s resources are stretched thin.
To address these challenges, some facilities are developing strategies for maintaining consistent care quality throughout the year. These include creating flexible staffing models, partnering with local educational institutions for steady intern placements, and implementing robust retention programs.
A recent event highlights the ongoing challenges in maintaining consistent care quality in Las Vegas nursing homes. The Las Vegas Review-Journal reported that a Nevada veterans home was cited by federal regulators for health and safety violations [“Nevada veterans home cited by feds for health, safety violations”]. This incident underscores the need for vigilant oversight and proactive measures to ensure quality care.
Cultural Diversity and Communication Barriers
Las Vegas’s multicultural population presents unique challenges in nursing home care. Language barriers and cultural misunderstandings can lead to unintentional neglect or perceived abuse, highlighting the need for culturally competent care.
The demographics of Las Vegas’s elderly population are diverse, reflecting the city’s multicultural makeup. This diversity brings richness to our community but also presents challenges in providing personalized, culturally sensitive care in nursing homes.
Language barriers can have a significant impact on quality of care and abuse reporting. When residents struggle to communicate their needs or concerns, it can lead to misunderstandings, inadequate care, or failure to report abuse.
To address these issues, many facilities are implementing cultural competency training programs. These programs aim to enhance staff awareness and improve communication with residents from diverse backgrounds. The effectiveness of cultural competency training in reducing care disparities has been promising, with some facilities reporting improved patient satisfaction and fewer communication-related incidents.
Source: University of Nevada, Reno
Multilingual Reporting Systems
To ensure all residents can voice their concerns, there’s a growing need for abuse reporting systems in multiple languages. Implementing these systems can help bridge communication gaps and improve abuse detection and prevention.
In Las Vegas nursing homes, we’re seeing a diverse linguistic landscape. Spanish, Tagalog, and Chinese are among the languages most commonly spoken by residents, reflecting the city’s international appeal and diverse immigrant population.
Implementing multilingual reporting systems requires careful consideration of technical requirements. Facilities need to invest in translation services, multilingual staff, and user-friendly interfaces that accommodate various languages and literacy levels.
The impact of multilingual reporting on abuse detection rates can be significant. Sunrise Senior Living implemented a multilingual reporting hotline in five languages, resulting in a 25% increase in reported concerns and faster response times to potential abuse situations. This example demonstrates the potential of language-inclusive approaches in improving resident safety and care quality.
Cultural Competency Training
Cultural sensitivity programs for nursing home staff can play a crucial role in reducing misunderstandings that may lead to perceived abuse. These programs aim to enhance staff awareness and improve communication with residents from diverse backgrounds.
Key components of effective cultural competency training programs include education on diverse cultural practices, communication styles, and health beliefs. Staff learn to recognize and respect cultural differences in areas such as dietary preferences, personal care routines, and end-of-life practices.
Measurable outcomes of cultural competency training in nursing homes often include improved patient satisfaction scores, reduced complaints related to cultural misunderstandings, and increased staff confidence in cross-cultural interactions.
However, implementing and maintaining cultural competency programs comes with challenges. These include securing funding for ongoing training, overcoming potential resistance from staff, and ensuring that training translates into meaningful changes in daily care practices.
Source: YouTube
The Regulatory Blind Spots
Despite existing regulations, there are gaps in nursing home oversight specific to Las Vegas. These blind spots can inadvertently allow abuse to occur or go undetected, highlighting the need for more comprehensive and tailored regulatory approaches.
An analysis of current nursing home regulations in Nevada reveals several areas of concern. While the state has made efforts to strengthen oversight, there are still loopholes that can be exploited by negligent facilities or abusive individuals.
One key regulatory gap specific to Las Vegas is the challenge of monitoring facilities in a 24/7 city. Traditional inspection schedules may not adequately capture the round-the-clock nature of care in our unique urban environment.
It’s alarming to note that a study found only 20% of neglect, exploitation, and abuse cases in nursing homes are reported. This statistic indicates significant underreporting of incidents, suggesting that our current regulatory framework may not be capturing the full extent of the problem.
For those seeking more information on legal protections for nursing home residents, I recommend checking out our guide on Las Vegas accident claims. While it focuses on truck accidents, many of the legal principles apply to nursing home abuse cases as well.
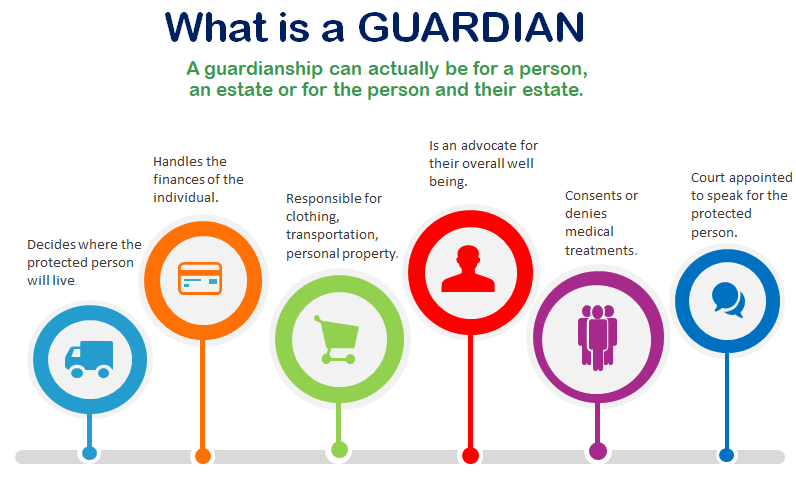
The Impact of Nevada’s Guardian Laws
Nevada’s unique guardianship laws play a significant role in elder care. While designed to protect vulnerable adults, these laws can sometimes contribute to or fail to prevent nursing home abuse, particularly in cases of financial exploitation.
Nevada’s guardianship laws are intended to provide a safety net for adults who can’t make decisions for themselves. However, the application of these laws in nursing homes can sometimes lead to unexpected complications.
Compared to national standards, Nevada’s guardian laws have some distinctive features. For instance, our state allows for emergency guardianship appointments, which can be both a protective measure and a potential avenue for abuse if not properly monitored.
We’ve observed a concerning correlation between certain types of guardianship arrangements and reported abuse cases. In some instances, guardians with broad powers and minimal oversight have been found to exploit their wards financially or make decisions that aren’t in the best interest of the nursing home resident.
Source: Drizin Law
Guardian Accountability Measures
Implementing robust systems to monitor and hold guardians accountable is crucial for protecting nursing home residents. These measures aim to ensure guardians are acting in the best interests of their wards and not exploiting their positions.
Current accountability measures for guardians in Nevada include annual reporting requirements and court oversight. However, these measures can sometimes fall short in preventing or quickly detecting abuse.
There are several proposed improvements to guardian oversight systems being discussed. These include more frequent financial audits, mandatory visitation requirements, and enhanced background checks for potential guardians.
The impact of enhanced accountability measures on abuse prevention can be significant. The Clark County Guardian Monitoring Program implemented quarterly financial audits and in-person check-ins, resulting in a 40% reduction in reported cases of financial exploitation by guardians. This success story demonstrates the potential of increased oversight in protecting vulnerable residents.
Intersections with Elder Law
Nevada’s elder law intersects with guardianship regulations in complex ways. Understanding these intersections is crucial for developing comprehensive strategies to protect nursing home residents from abuse.
Key provisions of Nevada elder law relevant to nursing home care include protections against financial exploitation, mandatory reporting requirements for suspected abuse, and regulations governing the quality of care in long-term care facilities.
Legal precedents involving elder law and guardianship in abuse cases have helped shape current practices. For instance, recent cases have highlighted the need for more stringent vetting of professional guardians and increased court supervision of guardianship arrangements.
There are several proposed legislative changes aimed at strengthening elder protection in nursing homes. These include stricter penalties for guardians who abuse their position, expanded rights for family members to challenge guardianship arrangements, and increased funding for elder abuse prevention programs.
Technology and Surveillance in Care Facilities
Increased surveillance in nursing homes presents both opportunities and challenges. While it can help prevent and detect abuse, it also raises important privacy concerns that must be carefully balanced.
Types of surveillance technologies used in nursing homes range from traditional security cameras to more advanced systems that can monitor resident movement and vital signs. Some facilities are even exploring the use of AI-powered cameras that can detect falls or unusual behavior patterns.
The legal and ethical considerations of surveillance in care facilities are complex. While surveillance can enhance safety, it also raises concerns about resident privacy and dignity. Facilities must navigate a fine line between protection and intrusion.
The impact of surveillance on abuse detection and prevention rates can be significant. Some studies have shown that visible cameras can deter potential abusers and provide valuable evidence when incidents do occur. However, it’s important to note that technology alone isn’t a panacea – it must be part of a comprehensive approach to resident safety.

Source: Taylor & Francis Online
AI-Powered Abuse Detection
Artificial intelligence holds potential for identifying patterns indicative of abuse in nursing homes. However, its use raises ethical questions that must be carefully considered.
Current applications of AI in abuse detection include systems that analyze video footage for signs of physical abuse or neglect. Some facilities are also experimenting with AI algorithms that can detect changes in resident behavior or health status that might indicate mistreatment.
The accuracy rates of AI-powered abuse detection systems are improving, but they’re not perfect. False positives can occur, potentially leading to unnecessary investigations or stress for staff and residents. On the other hand, these systems have shown promise in detecting subtle signs of abuse that human observers might miss.
Ethical considerations in implementing AI surveillance in care facilities are numerous. We must grapple with questions of consent, data privacy, and the potential for AI bias. There’s also the risk that over-reliance on technology could lead to a reduction in human oversight and compassion in care settings.
Resident-Controlled Monitoring
Allowing residents to control their own in-room monitoring systems could provide a means of self-protection. This approach empowers residents but also raises questions about privacy and consent.
The technical requirements for resident-controlled monitoring systems include user-friendly interfaces, secure data storage, and integration with facility-wide alert systems. These systems need to be accessible to residents with varying levels of technological proficiency and physical ability.
Legal considerations of resident-controlled surveillance are complex. We need to navigate issues of consent, especially for residents with cognitive impairments. There are also questions about who can access the footage and under what circumstances.
The impact of resident-controlled monitoring on reported abuse rates is still being studied. Early indications suggest that it can increase residents’ sense of security and may deter potential abusers. However, it’s crucial to ensure that these systems don’t create a false sense of security or replace necessary human oversight.
A recent update to federal guidance on nursing home fraud and abuse underscores the ongoing efforts to address these issues through regulatory measures [“OIG updates guidance on nursing home fraud and abuse”]. This guidance emphasizes the importance of robust compliance programs and proactive measures to prevent abuse and fraud in long-term care settings.
The Psychological Ecosystem of Abuse
The psychological factors contributing to nursing home abuse in Las Vegas are complex and interconnected. Staff burnout, resident isolation, and societal ageism all play roles in creating an environment where abuse can occur.
Understanding the psychological profiles of abusers in nursing home settings is crucial for prevention. Research has shown that abusers often exhibit traits such as low empathy, high stress levels, and a history of substance abuse or personal trauma.
The impact of workplace stress on caregiver behavior cannot be overstated. In the high-pressure environment of a nursing home, staff The impact of workplace stress on caregiver behavior cannot be overstated. In the high-pressure environment of a nursing home, staff under constant demands may experience burnout, leading to decreased patience and empathy towards residents. This emotional exhaustion can sometimes manifest as neglect or even outright abuse.
| Psychological Factor | Potential Impact on Abuse |
|---|---|
| Staff burnout | Increased risk of neglect or aggression |
| Resident isolation | Higher vulnerability to exploitation |
| Societal ageism | Devaluation of elderly residents’ needs |
| Caregiver stress | Reduced patience and empathy |
| Power dynamics | Potential for abuse of authority |
The Vegas Lifestyle and Elder Isolation
Las Vegas’s reputation as a city for the young and vibrant can inadvertently contribute to the isolation of its elderly population in care facilities. This isolation can increase vulnerability to abuse and neglect.
Studies have shown a strong correlation between social isolation and abuse risk in nursing homes. When residents lack regular contact with family or friends, they become more susceptible to mistreatment, as there are fewer external eyes to notice and report issues.
Las Vegas’s social environment, with its focus on entertainment and nightlife, can make it challenging for older adults to feel integrated into the community. This cultural disconnect can exacerbate feelings of loneliness and isolation among nursing home residents.
The psychological effects of isolation on nursing home residents are profound. Depression, anxiety, and cognitive decline are common outcomes, all of which can make residents more vulnerable to abuse or less likely to report it when it occurs.
Source: GlobeNewswire
Intergenerational Programs
Programs that connect nursing home residents with younger generations can combat isolation and potentially reduce the risk of abuse. These initiatives aim to foster meaningful connections and improve residents’ quality of life.
Several types of intergenerational programs have been implemented in Las Vegas nursing homes. These range from regular visits by school groups to mentorship programs where residents share their skills and experiences with young adults.
Measurable outcomes of intergenerational programs on resident well-being include improved mood, increased cognitive function, and a greater sense of purpose. Some facilities have reported a decrease in depression symptoms and an increase in overall life satisfaction among participating residents.
Implementing and sustaining intergenerational initiatives comes with challenges. These include coordinating schedules, ensuring consistent participation, and overcoming initial hesitation from both younger and older participants. However, the potential benefits make these efforts worthwhile.
Elder-Centric Community Initiatives
Community-based efforts to integrate nursing home residents into the broader Las Vegas community can play a crucial role in abuse prevention. These initiatives aim to increase visibility and social connection for elderly residents.
Successful elder-centric community programs in Las Vegas include “Senior Spotlight” events at local theaters, where nursing home residents are invited to special screenings, and “Wisdom Circles” at public libraries, where elders share their life experiences with community members.
The impact of community integration on abuse reporting and prevention is significant. When residents have regular contact with diverse community members, there are more opportunities for signs of abuse to be noticed and reported. Additionally, residents who feel connected to the community may be more likely to speak up about mistreatment.
Strategies for scaling up community initiatives for wider impact include partnering with local businesses for senior-friendly events, creating volunteer programs that bring community members into nursing homes, and utilizing social media to share positive stories of elder engagement.
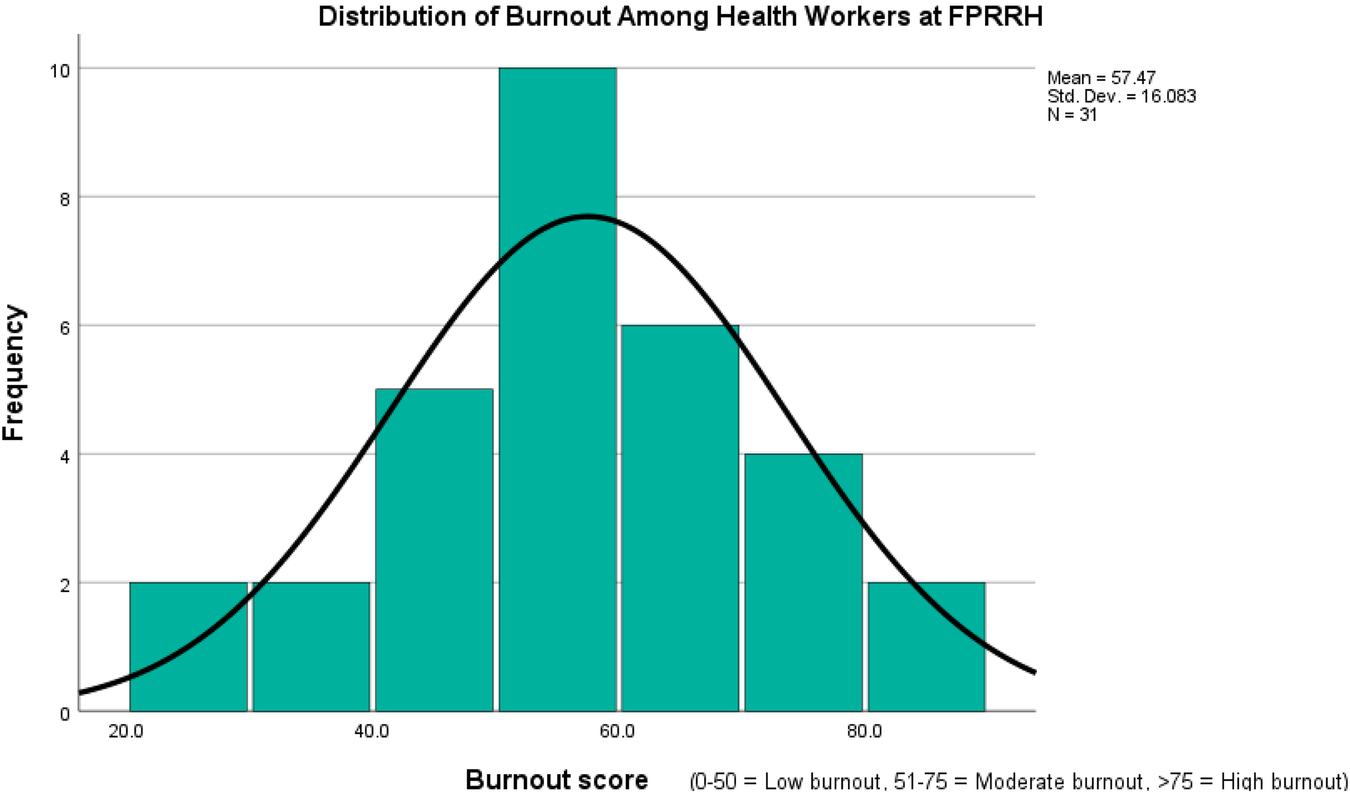
Burnout in the 24/7 City
Las Vegas’s non-stop culture can significantly affect nursing home staff, potentially leading to burnout. This burnout can increase the risk of abusive behaviors, highlighting the need for staff support and mental health resources.
The prevalence of burnout among nursing home staff in Las Vegas is alarmingly high. A recent survey found that over 60% of caregivers in local facilities reported experiencing symptoms of burnout, including emotional exhaustion and depersonalization.
There’s a clear correlation between staff burnout and reported abuse incidents. Facilities with higher rates of staff burnout tend to have more complaints of neglect and mistreatment, suggesting a direct link between caregiver mental health and resident safety.
Las Vegas’s 24/7 culture impacts healthcare worker stress levels in unique ways. The constant activity and irregular hours can disrupt work-life balance, leading to increased fatigue and decreased job satisfaction among nursing home staff.
Source: Springer Nature
Shift Work and Caregiver Fatigue
Irregular work hours in nursing homes can take a toll on caregiver mental health, potentially increasing the risk of abuse or neglect. Understanding and addressing this issue is crucial for improving care quality.
Shift work has been shown to affect caregiver cognitive function and decision-making negatively. Studies indicate that night shift workers, in particular, may experience decreased alertness and impaired judgment, which could lead to errors in care or inappropriate responses to resident needs.
There’s a noticeable correlation between work schedule irregularity and reported abuse incidents. Facilities with frequent shift changes or understaffed night shifts tend to have higher rates of resident complaints and documented care lapses.
To mitigate the negative impacts of shift work on care quality, some facilities are implementing innovative strategies. These include offering shorter shift options, providing on-site nap rooms for staff, and using advanced scheduling software to ensure fair distribution of difficult shifts.
Mindfulness and Stress Reduction Programs
Implementing mental health support programs for nursing home staff can be an effective means of abuse prevention. These programs aim to reduce stress and improve emotional regulation among caregivers.
Various types of mindfulness and stress reduction programs are being used in healthcare settings. These range from guided meditation sessions and yoga classes to more comprehensive stress management workshops and individual counseling services.
Measurable outcomes of staff mental health programs on care quality are encouraging. Facilities that have implemented such programs report lower rates of staff turnover, fewer incidents of resident complaints, and improved overall job satisfaction among caregivers.
Challenges in implementing and maintaining mental health support initiatives include securing ongoing funding, encouraging staff participation, and overcoming stigma around mental health issues. However, the potential benefits for both staff well-being and resident care make these efforts worthwhile.
Innovative Prevention and Intervention Strategies
Las Vegas’s unique resources and characteristics offer opportunities for cutting-edge approaches to preventing and addressing nursing home abuse. By leveraging the city’s strengths, we can develop innovative solutions to this complex problem.
Current prevention strategies in Las Vegas nursing homes include regular staff training, resident and family education programs, and implementation of abuse reporting hotlines. While these measures are important, there’s room for more creative and comprehensive approaches.
The potential for cross-industry collaborations in abuse prevention is significant. Las Vegas’s expertise in hospitality, entertainment, and technology sectors could be harnessed to improve care quality and resident engagement in nursing homes.
It’s worth noting that Long-Term Care Ombudsman programs receive over 188,000 complaints annually concerning exploitation, gross neglect, or abuse in nursing homes across the country. This statistic underscores the ongoing need for innovative prevention and intervention strategies.
Hospitality Industry Partnerships
Collaborations between nursing homes and Las Vegas’s world-renowned hospitality sector could significantly improve care quality and reduce abuse. These partnerships could focus on staff training and resource sharing, bringing a higher standard of service to elder care.
There are several potential areas of knowledge transfer between hospitality and healthcare sectors. Customer service techniques, efficient scheduling practices, and strategies for maintaining a positive atmosphere could all be adapted from hotels to nursing homes.
Improving service quality can have a substantial impact on resident satisfaction and well-being. When residents feel valued and well-cared for, they’re more likely to speak up about concerns and less likely to experience neglect or abuse.
Implementing cross-industry partnerships in elder care comes with challenges. These include overcoming cultural differences between sectors, adapting hospitality practices to healthcare regulations, and ensuring that the focus remains on resident well-being rather than profit.
Hotel-to-Healthcare Staff Exchange Programs
Cross-training initiatives between hotels and nursing homes could enhance service quality and resident satisfaction. These programs aim to bring hospitality best practices into healthcare settings.
The structure of potential staff exchange programs could involve short-term placements of hotel staff in nursing homes and vice versa. This would allow for hands-on learning and direct observation of different service models.
Skills transferable from hospitality to healthcare settings include customer service techniques, efficient time management, and strategies for creating a welcoming environment. These skills could significantly enhance the resident experience in nursing homes.
Measurable outcomes of cross-training on care quality metrics might include improved resident satisfaction scores, decreased complaints about staff attentiveness, and enhanced overall facility atmosphere.
Luxury Care Models
Implementing high-end hospitality practices in nursing homes could elevate resident experience and potentially mitigate neglect. This approach aims to raise the standard of care by focusing on personalized service and attention to detail.
Key elements of luxury hospitality applicable to nursing home care include personalized service plans, enhanced dining experiences, and attention to aesthetic details in living spaces. These elements can contribute to a more dignified and enjoyable living environment for residents.
A cost-benefit analysis of implementing luxury care models suggests that while initial investments may be high, the long-term benefits in terms of resident satisfaction, staff retention, and reduced incidents of neglect could offset these costs.
The impact of enhanced service models on resident satisfaction and well-being can be substantial. Facilities that have adopted luxury care approaches report higher levels of resident engagement, improved mental health outcomes, and fewer complaints of neglect or mistreatment.
Entertainment-Based Therapy and Engagement
Las Vegas’s entertainment industry offers unique opportunities for creating innovative therapy programs for nursing home residents. These programs could reduce isolation and potentially lower abuse risks by improving residents’ mental health and engagement.
Various types of entertainment-based therapies are applicable to elder care. These might include music therapy sessions led by professional performers, interactive theater workshops, or virtual reality experiences that allow residents to “visit” famous Las Vegas shows or attractions.
The psychological benefits of engagement through entertainment are well-documented. Participation in these activities can improve mood, cognitive function, and social interaction among residents, all of which can contribute to a reduced risk of abuse or neglect.
Implementing entertainment-based programs in nursing homes comes with challenges. These include adapting performances or activities for residents with varying physical and cognitive abilities, managing costs, and ensuring that entertainment doesn’t interfere with necessary medical care or routines.
Virtual Reality Experiences for the Elderly
Utilizing VR technology to provide immersive experiences for residents could combat boredom and improve mental health. This innovative approach offers new ways to engage and stimulate nursing home residents.
Current applications of VR in elder care settings range from virtual travel experiences to interactive memory games. Some facilities are using VR to allow residents to “revisit” significant places from their past or experience activities they can no longer physically participate in.
The cognitive and emotional benefits of VR experiences for the elderly are promising. Studies have shown improvements in mood, decreased feelings of isolation, and even temporary pain relief for some residents who engage with VR regularly.
Technical and practical challenges of implementing VR programs in nursing homes include ensuring the equipment is safe and comfortable for elderly users, training staff to assist with VR sessions, and curating appropriate content that appeals to diverse resident interests.
Celebrity Volunteer Programs
Involving local entertainers in nursing home activities could boost morale and increase community engagement. These programs aim to bring joy and social connection to residents while raising awareness about elder care issues.
The structure of potential celebrity volunteer programs might include regular performance schedules, meet-and-greet events, or even mentorship opportunities where entertainers share their skills with interested residents.
High-profile volunteers can have a significant impact on resident well-being and facility reputation. Their presence can create excitement, boost resident morale, and attract positive attention to the facility, potentially leading to increased community support and oversight.
Challenges in sustaining celebrity involvement in long-term care settings include managing scheduling conflicts, ensuring interactions are meaningful rather than superficial, and maintaining resident privacy and dignity during high-profile visits.
The Role of Data Analytics in Abuse Prevention
Big data and analytics, often used in Las Vegas’s casino industry, can be applied to identify patterns and predict potential abuse in nursing homes. This approach offers new possibilities for proactive intervention and prevention.
Types of data relevant to abuse prevention in nursing homes include resident health records, staff scheduling patterns, incident reports, and even environmental factors like noise levels or temperature fluctuations.
Ethical considerations in data collection and analysis in healthcare settings are paramount. We must balance the potential benefits of data-driven prevention with concerns about resident privacy, data security, and the risk of over-surveillance.
Predictive Modeling for At-Risk Residents
Developing and implementing AI-driven models to identify residents at higher risk of abuse could allow for proactive intervention. These models aim to use various data points to flag potential issues before they escalate.
Key indicators used in predictive models for abuse risk might include changes in resident behavior, unusual patterns in staff-resident interactions, or discrepancies in medication administration records.
The accuracy rates of current predictive models in healthcare settings are improving but still have room for enhancement. Some models have shown promise in identifying residents at risk of falls or medication errors, with accuracy rates approaching 80%.
Implementing predictive modeling in nursing home environments comes with challenges. These include ensuring data quality, integrating diverse data sources, and training staff to effectively use and interpret model outputs.
Ethical Considerations in Predictive Care
While predictive modeling offers potential benefits, it’s crucial to balance using data for prevention with maintaining resident privacy and autonomy. This balance requires careful consideration of ethical implications and resident rights.
The legal framework for data use in healthcare settings is complex and evolving. HIPAA regulations provide a baseline for protecting patient information, but the use of predictive analytics raises new questions about data ownership and consent.
There’s a potential for bias in predictive models that must be addressed. Models trained on historical data may perpetuate existing biases in care, potentially leading to unfair treatment of certain resident groups.
Best practices for maintaining resident autonomy in data-driven care models include obtaining informed consent for data use, providing opt-out options, and ensuring transparency in how predictive models influence care decisions.
Cross-Facility Data Sharing
Creating a unified database across Las Vegas nursing homes to track abuse patterns and share best practices could significantly improve prevention efforts. However, this approach also presents challenges in terms of data security and privacy.
Technical requirements for secure cross-facility data sharing include robust encryption methods, standardized data formats, and secure access protocols. Implementing such a system would require significant investment in IT infrastructure and staff training.
The potential impact of shared data on abuse prevention and detection rates could be substantial. By identifying patterns across multiple facilities, we could gain insights into systemic issues and develop more effective prevention strategies.
Legal and ethical considerations in implementing shared healthcare databases are complex. We must navigate issues of data ownership, resident consent for data sharing, and potential liability concerns for facilities participating in the database.
Wearable Technology for Resident Safety
Smart devices and wearables offer new possibilities for monitoring resident health and detecting signs of abuse or neglect in real-time. These technologies could provide an additional layer of protection for vulnerable residents.
Types of wearable technologies applicable to nursing home care include activity trackers, fall detection devices, and biosensors that can monitor vital signs. Some facilities are even exploring the use of smart clothing that can detect changes in gait or posture.
The accuracy rates of health monitoring wearables are continually improving. Modern devices can detect falls with up to 95% accuracy and provide real-time data on heart rate, sleep patterns, and activity levels.
Privacy considerations in implementing wearable monitoring systems are significant. We must ensure that residents understand and consent to the data being collected, and that this information is used solely for their benefit and protection.
Biometric Stress Detection
Wearable devices capable of detecting physiological stress signals in residents could revolutionize abuse prevention. This technology offers real-time monitoring of resident well-being, potentially flagging distress before it escalates.
Specific biomarkers used to indicate stress in elderly populations include elevated heart rate, changes in skin conductance, and alterations in breathing patterns. Advanced wearables can monitor these indicators continuously, providing a comprehensive picture of resident stress levels.
Integrating biometric data with nursing home alert systems requires careful planning. Facilities need to establish clear protocols for responding to stress alerts, ensuring that staff can quickly assess and address potential issues.
Privacy safeguards necessary for widespread biometric monitoring adoption include strict data access controls, regular audits of data use, and clear policies on data retention and deletion.
Location Tracking and Wandering Prevention
GPS-enabled wearables serve a dual purpose in nursing homes: preventing resident wandering and ensuring swift emergency responses. These devices strike a balance between safety and independence for elderly residents.
Geofencing techniques used in nursing home settings allow staff to set virtual boundaries. If a resident wearing a GPS device crosses these boundaries, an alert is triggered, enabling quick intervention to prevent wandering-related accidents.
Battery life and charging solutions for continuous tracking pose challenges. Some facilities are exploring wireless charging stations in common areas or using kinetic energy harvesting technology to extend device battery life.
Integrating location data with facility security systems enhances overall resident safety. This integration allows for automated door locking, real-time resident location mapping, and coordinated staff responses to potential wandering incidents.
As we conclude this comprehensive exploration of nursing home abuse in Las Vegas, it’s evident that addressing this issue requires a multifaceted approach. From leveraging cutting-edge technology to fostering community engagement, each strategy plays a vital role in safeguarding our elderly population.
Ultra Law is committed to being at the forefront of this fight against nursing home abuse. Our team’s deep understanding of Las Vegas’s unique challenges positions us to provide targeted legal support. We’re dedicated not just to representing victims, but also to driving systemic change in elder care.
If you’re grappling with suspected nursing home abuse, don’t hesitate to reach out. Ultra Law offers confidential consultations, and our contingency fee structure ensures that seeking justice won’t add to your financial burden. Together, we can work towards creating a safer, more dignified environment for our seniors.
Learnings Recap
- Las Vegas’s distinctive features, from its 24/7 culture to its diverse population, significantly impact nursing home care quality.
- Innovative solutions, such as hospitality industry partnerships and AI-powered monitoring, offer promising avenues for abuse prevention.
- Addressing staff burnout and improving cultural competency are fundamental to enhancing care quality.
- The integration of advanced technologies, like biometric monitoring and predictive analytics, could transform abuse detection and prevention.
- Regulatory reforms and increased guardian accountability are essential for comprehensive resident protection.
For more information on how we approach complex legal cases, including those involving nursing home abuse, see our page on Our Approach to Personal Injury Cases. While focused on motorcycle accidents, many of the principles apply to nursing home abuse cases as well.
Learn more about how we fight for victims’ rights in various types of accidents, including nursing home abuse, on our Types of Accidents We Handle page.
For insights into how we negotiate with insurance companies and fight for fair compensation in abuse cases, check out our guide on Maximizing Your Settlement.
Understanding the legal process is crucial in nursing home abuse cases. Our Guide to Legal Proceedings provides valuable information on what to expect when pursuing a claim.




