In 2023, medical malpractice payouts in the United States hit a whopping $4.03 billion, jumping up 22% from the year before. That’s not just a number—it’s a wake-up call. I’ve seen firsthand how these cases can turn lives upside down. My neighbor, a retired nurse, went through hell with a misdiagnosis that led to unnecessary surgery. Her story stuck with me, and it’s why I’m diving deep into medical malpractice settlements for 2024.
Whether you’re a patient worried about your care, a healthcare provider trying to protect yourself, or a legal eagle looking to stay sharp, understanding these settlements is crucial. I’m here to break it all down for you—from what counts as negligence to the nitty-gritty of negotiating a fair deal. By the time we’re done, you’ll have the know-how to tackle medical malpractice issues head-on.
Let’s get one thing straight: medical malpractice isn’t just about doctors making mistakes. It’s a complex legal beast that can bite when you least expect it. In 2024, we’re seeing new twists and turns in how these cases play out. I’ll guide you through the maze, showing you what to watch for and how to protect your rights.
Learn more about our approach to handling accident cases and how it applies to medical malpractice.
:max_bytes(150000):strip_icc()/malpractice-insurance_final-2175f546cee84786bcfb014a03ee4a1b.png)
Understanding Medical Malpractice
Medical malpractice is no joke. It’s what happens when healthcare professionals drop the ball, and patients pay the price. We’re talking about situations where doctors, nurses, or other medical staff fail to provide proper care, leading to harm or even death. In 2024, the landscape is shifting, and it’s more important than ever to know what constitutes malpractice.
Here’s the deal: not every bad outcome in healthcare is malpractice. Sometimes, treatments just don’t work out despite everyone’s best efforts. But when a healthcare provider’s actions (or lack thereof) fall below the accepted standard of care, that’s when we enter malpractice territory. It’s a fine line, and it’s one that courts and lawyers spend a lot of time arguing over.
The stakes are high in these cases. We’re not just talking about money—though that’s certainly part of it. We’re talking about people’s lives, their health, and their futures. That’s why it’s crucial to understand what malpractice looks like and how it’s handled in the legal system.
Discover how our commitment to clients extends to medical malpractice cases.
Defining Medical Negligence
Let’s get into the nitty-gritty of medical negligence. It’s the heart of any malpractice claim, but it’s not as simple as saying, “The doctor messed up.” Medical negligence has a specific legal definition, and it’s all about proving that a healthcare provider failed to meet the standard of care expected in their field.
To break it down, we’re looking at four key elements: duty, breach, causation, and damages. First, there needs to be a duty of care—basically, the doctor-patient relationship has to exist. Then, we need to show that the provider breached that duty by doing something (or not doing something) that a reasonable professional in their position would have done differently.
But it doesn’t stop there. We also need to prove that this breach directly caused harm to the patient. And finally, we need to show that the patient suffered actual damages as a result. It’s like a legal puzzle, and all the pieces need to fit for a malpractice claim to hold water.
Elements of Negligence
Let’s dive deeper into these elements of negligence. They’re the building blocks of any medical malpractice case, and understanding them is key to figuring out if you’ve got a valid claim on your hands.
First up is duty of care. This is established when you become a patient under a healthcare provider’s care. It’s pretty straightforward—if you’re seeing a doctor for treatment, they owe you a duty of care. Next, we’ve got breach of duty. This is where things can get tricky. It’s not enough for something to go wrong; we need to show that the provider’s actions fell below the accepted standard in their field. This often requires expert testimony to establish what that standard is and how it was breached.
Causation is where many malpractice cases live or die. It’s not enough to show that a mistake was made; we need to prove that the mistake directly led to the patient’s injury or harm. This can be challenging, especially in complex medical cases where multiple factors might be at play. Finally, we have damages. These can be economic (like medical bills or lost wages) or non-economic (like pain and suffering). Without provable damages, there’s no case, no matter how egregious the medical error might have been.
| Element | Description |
|---|---|
| Duty of Care | Established doctor-patient relationship |
| Breach of Duty | Actions deviating from accepted standards |
| Causation | Direct link between breach and injury |
| Damages | Quantifiable harm (financial, physical, emotional) |
Common Types of Medical Malpractice
Now, let’s talk about the types of medical malpractice we’re seeing most often in 2024. Misdiagnosis tops the list, and it’s not hard to see why. With complex symptoms and time pressures, doctors sometimes miss the mark. But when a misdiagnosis leads to improper treatment or delayed care, the consequences can be severe.
Surgical errors are another big one. We’re talking wrong-site surgeries, leaving instruments inside patients, or even performing the wrong procedure altogether. It sounds like something out of a horror movie, but it happens more often than you’d think. Medication mistakes round out the top three—wrong dosages, drug interactions, or prescribing the wrong medication can all have serious consequences.
Birth injuries are a particularly heartbreaking category of malpractice. These cases often involve lifelong consequences for both the child and the family. Whether it’s a failure to monitor fetal distress or improper use of delivery tools, the results can be devastating.
According to the “Medical Malpractice Report,” a whopping 34.1% of medical malpractice actions were related to diagnostic errors, making it the most common type of claim. That’s a third of all cases stemming from misdiagnosis or delayed diagnosis. It’s a stark reminder of how crucial accurate and timely diagnoses are in healthcare.
Statute of Limitations
Time is not on your side when it comes to medical malpractice claims. Each state has its own statute of limitations, and if you miss that deadline, you’re out of luck—no matter how strong your case might be. These time limits exist for good reasons, like ensuring evidence is still fresh and protecting healthcare providers from endless liability. But they can also be a major hurdle for patients who might not immediately realize they’ve been victims of malpractice.
In most states, the clock starts ticking from the date of the alleged malpractice. But it’s not always that simple. Some states have a “discovery rule” that extends the deadline if the patient couldn’t reasonably have known about the malpractice right away. And for minors, the rules can be different, often allowing more time to file a claim.
Understanding time limits for accident claims is equally important in medical malpractice cases.
Discovery Rule
The discovery rule is a game-changer in medical malpractice law. It recognizes that some injuries or errors might not be immediately apparent. Instead of starting the clock on the statute of limitations from the date of the malpractice, it begins when the patient discovers (or reasonably should have discovered) that they were harmed by medical negligence.
This rule can be a lifeline for patients who don’t immediately connect their health issues to a past medical procedure or treatment. For example, if a surgeon leaves a sponge inside a patient during surgery, the patient might not realize it for months or even years. The discovery rule allows them to pursue a claim when they finally uncover the problem, rather than being barred by a statute of limitations that expired before they even knew there was an issue.
But here’s the catch: the discovery rule isn’t a blank check to file whenever you want. Courts will look at when a reasonable person should have discovered the malpractice. If you ignored obvious symptoms or failed to follow up on clear red flags, you might still find yourself out of luck.
A recent Illinois case, Larson v. Crosby, really drives home how tricky these timing issues can be. The Appellate Court overturned a lower court’s decision that had thrown out a malpractice case based on the statute of limitations. They said there were still questions about when the clock should have started ticking. It just goes to show how complex these timing issues can be in medical malpractice cases.
Initiating a Medical Malpractice Claim
So, you think you’ve got a medical malpractice case on your hands. What now? Initiating a claim isn’t as simple as marching into a lawyer’s office and demanding justice. It’s a complex process that requires careful planning and execution. Let’s break it down step by step.
First things first: you need to gather all your medical records. And I mean all of them. Every doctor’s visit, every prescription, every test result—it all matters. This is the foundation of your case, and you can’t afford to leave anything out. Next, you’ll want to get a medical expert on board. Most states require an expert opinion just to file a claim, so this isn’t something you can skip.
Once you’ve got your ducks in a row, it’s time to think about pre-litigation requirements. Many states have specific hoops you need to jump through before you can file a lawsuit. This might include sending a notice of intent to sue or going through a medical review panel. Skip these steps, and your case could be dead in the water before it even starts.

Gathering Evidence
Evidence is the lifeblood of any medical malpractice claim. Without solid proof, you’re just spinning your wheels. So what kind of evidence are we talking about? Medical records are the obvious starting point, but that’s just the tip of the iceberg.
You’ll want to collect any correspondence with healthcare providers, including emails or text messages. If you kept a journal of your symptoms or treatment, that can be gold. Photos or videos of your condition can be powerful evidence, especially if you’re dealing with visible injuries or symptoms.
Don’t forget about witness statements. Anyone who saw your condition before, during, or after the alleged malpractice could be crucial to your case. This might include family members, friends, or even other healthcare providers who treated you.
Medical Expert Affidavits
Let’s talk about medical expert affidavits. These aren’t just nice-to-have documents—in many states, they’re absolutely essential to even get your foot in the door with a malpractice claim. An affidavit is basically a sworn statement from a qualified medical expert saying that your case has merit.
The expert needs to review your medical records and state that, in their professional opinion, the care you received fell below the accepted standard. They’ll need to explain how the healthcare provider’s actions (or inactions) caused your injury or harm. It’s not enough for them to say, “Yeah, this looks bad.” They need to provide specific details and reasoning.
Getting the right expert is crucial. You want someone with credentials in the same field as the provider you’re suing. If you’re claiming a surgeon messed up, you need a surgeon to back you up—not a general practitioner or a nurse, no matter how experienced they might be.
The Illinois Supreme Court recently shook things up a bit with their ruling in Cleeton v. SIU Healthcare. They said that at the early stages of a case, plaintiffs only need to show “probable cause” that there might be liability. This is a lower bar than proving definitive malpractice right out of the gate. It’s a change that could make it easier for valid claims to move forward in the legal system.
Documenting Economic and Non-Economic Damages
When it comes to damages in medical malpractice cases, we’re looking at two main categories: economic and non-economic. Economic damages are the straightforward ones—medical bills, lost wages, future medical care costs. These are the numbers you can point to and say, “Look, this is what this mistake cost me in dollars and cents.”
Non-economic damages are trickier. We’re talking about pain and suffering, emotional distress, loss of enjoyment of life. How do you put a price tag on not being able to play with your kids or pursue your hobbies? It’s not easy, but it’s a crucial part of many malpractice claims.
For economic damages, keep every bill, every receipt, every pay stub. If you had to hire help around the house because of your injury, keep those records too. For future costs, you might need expert testimony to project ongoing medical needs or lost earning capacity.
Non-economic damages require a different approach. Keep a journal documenting how the injury affects your daily life. Get statements from friends and family about how they’ve seen you change. Psychological evaluations can also be powerful evidence of emotional distress.
| Type of Damage | Examples | Documentation Methods |
|---|---|---|
| Economic | Medical bills, lost wages | Receipts, pay stubs, expert projections |
| Non-Economic | Pain and suffering, emotional distress | Personal journals, psychological evaluations |
Pre-Litigation Requirements
Before you can storm the courthouse steps with your malpractice claim, many states require you to jump through some hoops. These pre-litigation requirements are designed to weed out frivolous lawsuits and encourage early settlements. They can be a pain, but ignore them at your peril—failing to meet these requirements can get your case tossed out before it even starts.
Some states require you to submit your claim to a medical review panel before filing a lawsuit. These panels, usually made up of healthcare professionals, review the evidence and give an opinion on whether malpractice occurred. Their decision isn’t binding, but it can be powerful evidence if your case goes to trial.
Other states mandate mediation or other forms of alternative dispute resolution before you can file suit. The idea is to get both sides talking and potentially reach a settlement without clogging up the court system. Even if you don’t settle, these sessions can give you valuable insights into the other side’s position.

Notice of Intent to Sue
In many states, you can’t just ambush a healthcare provider with a lawsuit. You’ve got to give them a heads-up first, and that’s where the Notice of Intent to Sue
Notice of Intent to Sue
In many states, you can’t just ambush a healthcare provider with a lawsuit. You’ve got to give them a heads-up first, and that’s where the Notice of Intent to Sue comes into play. This formal document is your way of saying, “Hey, I’m about to sue you, and here’s why.” It’s not just a courtesy—it’s often a legal requirement.
The notice typically needs to include specific details about your claim. We’re talking names of all the healthcare providers involved, a description of the alleged malpractice, and the harm you suffered as a result. Some states even require you to outline the legal basis for your claim.
Timing is crucial here. Most states have strict deadlines for when this notice needs to be sent. Miss the deadline, and you could lose your right to sue altogether. On the flip side, sending the notice often pauses the statute of limitations clock, giving you more time to build your case.
Filing the Lawsuit
If pre-litigation efforts don’t pan out, it’s time to roll up your sleeves and file that lawsuit. This is where the rubber meets the road in your malpractice claim. Filing a lawsuit isn’t just about paperwork—it’s a strategic move that sets the tone for your entire case.
First, you’ll need to choose the right court. Medical malpractice cases usually end up in state court, but there are exceptions. If you’re suing a federal healthcare provider, for instance, you might find yourself in federal court.
Once you’ve picked your battlefield, it’s time to draft the complaint. This document lays out your case in detail—who did what, when they did it, and how it harmed you. It’s not the place for flowery language or emotional appeals. Stick to the facts, and make sure every allegation ties back to the elements of medical malpractice we talked about earlier.
![How eFiling works [infographic] - One Legal](https://onelegal.com/wp-content/uploads/2018/10/HoweFilingworks_10.17.18.png)
Complaint and Summons
The complaint is your opening salvo in the legal battle. It’s a formal document that spells out your case against the healthcare provider. You’ll need to identify all the defendants—and in a medical malpractice case, there might be quite a few. Think doctors, nurses, hospitals, and even medical device manufacturers.
In your complaint, you’ll lay out the facts of your case and explain how they add up to malpractice. You’ll also need to specify what kind of damages you’re seeking. Be careful here—some states have specific requirements about how damages should be listed in a malpractice complaint.
Along with the complaint, you’ll file a summons. This is the court’s way of officially notifying the defendants that they’re being sued. It tells them how long they have to respond and what happens if they don’t.
Once you’ve filed these documents with the court, you’re not done yet. You’ve got to serve them on the defendants. This usually means hiring a process server to physically deliver the papers. It’s a crucial step—if you mess up service, the defendants could get the case thrown out on a technicality.
Negotiating Medical Malpractice Settlements
Alright, you’ve filed your lawsuit. Now what? In most cases, you’re not heading straight to trial. Instead, you’re entering the complex world of settlement negotiations. This is where the real action happens in medical malpractice cases.
Settlement talks can kick off at any point in the legal process. Sometimes, they start as soon as the defendant gets that notice of intent to sue. Other times, they heat up after discovery, when both sides have had a chance to see the evidence.
These negotiations are a delicate dance. You’re trying to get fair compensation for your injuries, while the other side is looking to minimize their payout. It’s not just about throwing numbers back and forth—it’s about building a compelling case for why you deserve what you’re asking for.
Remember, settling isn’t a sign of weakness. Even if you’ve got a rock-solid case, trials are expensive, time-consuming, and unpredictable. A good settlement can get you fair compensation without the stress and uncertainty of a trial.
Learn about our approach to negotiation and how we fight for our clients’ rights.
Factors Influencing Settlement Amounts
When it comes to settlement amounts, there’s no one-size-fits-all formula. Each case is unique, and a variety of factors can push the numbers up or down. Understanding these factors is key to setting realistic expectations and negotiating effectively.
The severity of your injury is a major player here. Permanent disabilities or life-altering conditions typically lead to higher settlements than temporary injuries. The impact on your ability to work and enjoy life also weighs heavily.
The strength of your evidence matters too. If you’ve got clear-cut proof of negligence and a rock-star expert witness, you’re in a stronger position to demand a higher settlement. On the flip side, if there are holes in your case or conflicting expert opinions, the defense might push for a lower number.
Your jurisdiction can also play a role. Some areas are known for being more plaintiff-friendly, while others tend to favor healthcare providers. Historical data on verdicts and settlements in your area can give you a sense of what to expect.
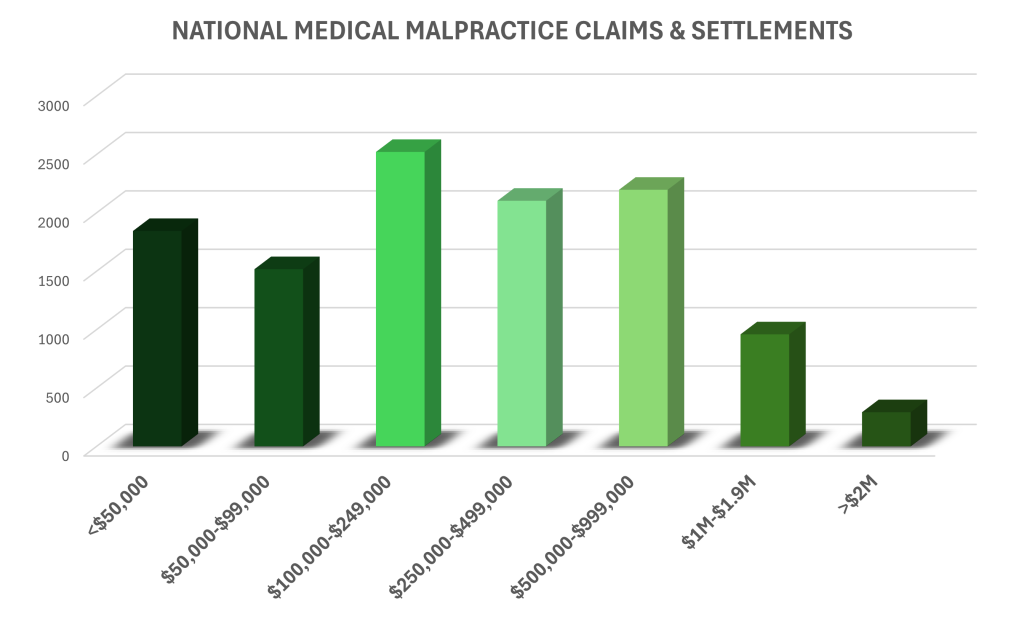
According to the “Medical Malpractice Report,” claims involving brain damage have seen payouts up to $960,000—significantly higher than the average. This underscores how the nature and severity of the injury can dramatically impact settlement amounts.
Severity of Injury
The severity of your injury is often the biggest factor in determining settlement amounts. It’s not just about the immediate medical costs—it’s about the long-term impact on your life. Permanent disabilities, chronic pain, or the need for ongoing care can all drive up settlement values.
Brain injuries, for instance, often result in some of the highest settlements. They can affect every aspect of a person’s life, from their ability to work to their relationships with family and friends. Spinal cord injuries are another category that tends to see high settlements, especially if they result in paralysis.
But it’s not just about physical injuries. Psychological trauma can also play a significant role in settlement negotiations. PTSD, depression, or anxiety resulting from medical malpractice can have a profound impact on a person’s quality of life.
It’s worth noting that the most severe injuries don’t always lead to the highest settlements. Sometimes, cases involving wrongful death can result in lower payouts than those involving severe, long-term disabilities. This is because ongoing medical care and lost earning capacity over a lifetime can add up to more than the damages typically awarded in wrongful death cases.
Quality of Evidence
In the world of medical malpractice settlements, evidence is king. The strength and quality of your evidence can make or break your case, and it plays a huge role in determining settlement amounts. Strong evidence can pressure defendants into offering higher settlements to avoid the risk of losing at trial.
Medical records are the foundation of your evidence. Clear documentation of errors, inconsistencies in treatment notes, or records showing a failure to follow standard protocols can be powerful ammunition in settlement negotiations. But it’s not just about having the records—it’s about how they’re interpreted and presented.
Expert testimony is another crucial piece of the puzzle. A well-respected expert who can clearly explain how the healthcare provider’s actions fell below the standard of care can significantly boost your bargaining power. On the flip side, if the defense has equally credible experts contradicting your claims, it could weaken your position.
Physical evidence can also be compelling. X-rays showing surgical errors, photographs documenting the progression of an injury, or video evidence of a patient’s changed physical capabilities can all strengthen your case.
Remember, it’s not just about quantity—quality matters. A few pieces of rock-solid evidence can be more valuable than a mountain of circumstantial or weak evidence. Your legal team’s ability to present this evidence effectively, tying it all together into a coherent narrative of negligence and harm, can significantly impact your settlement prospects.
Jurisdiction Tendencies
Where you file your lawsuit can have a big impact on your settlement prospects. Different jurisdictions have different track records when it comes to medical malpractice cases, and savvy attorneys on both sides are well aware of these tendencies.
Some areas are known for being more plaintiff-friendly, with juries that tend to award higher damages. In these jurisdictions, defendants might be more willing to offer generous settlements to avoid the risk of a trial. Other areas have reputations for being more sympathetic to healthcare providers, which could lead to lower settlement offers.
It’s not just about jury tendencies, though. Some jurisdictions have specific laws or court rules that can affect malpractice cases. For example, some states have caps on non-economic damages, which can limit the potential payout in a case. Others have specific pre-trial procedures that can impact the timeline and cost of litigation.
The local legal community plays a role too. In smaller jurisdictions, attorneys and judges may be more familiar with each other, which can influence how cases are handled. The reputation of local law firms and individual attorneys can also factor into settlement negotiations.
Keep in mind that these jurisdictional tendencies aren’t set in stone. They can change over time due to shifts in public opinion, changes in local laws, or even high-profile cases that set new precedents. A good legal team will stay on top of these trends and adjust their strategy accordingly.
Mediation and Alternative Dispute Resolution
Mediation and other forms of alternative dispute resolution (ADR) have become increasingly popular in medical malpractice cases. These methods offer a way to resolve disputes without the time, expense, and uncertainty of a full-blown trial.
In mediation, a neutral third party helps facilitate negotiations between you and the healthcare provider (or their insurance company). The mediator doesn’t make decisions or force agreements—their job is to help both sides find common ground and work towards a mutually acceptable solution.
ADR can take other forms too. Arbitration, for instance, is more formal than mediation. An arbitrator or panel of arbitrators hears evidence from both sides and makes a binding decision. Some healthcare contracts include mandatory arbitration clauses, so it’s worth checking if this applies to your case.
These methods can be particularly useful in complex medical malpractice cases. They allow for more nuanced discussions about liability and damages than you might get in a courtroom setting. They also offer more flexibility in terms of outcomes—you’re not limited to just monetary damages, for instance.
Benefits of Mediation
Mediation offers a unique set of advantages in medical malpractice cases. For starters, it’s usually faster and less expensive than going to trial. You can often schedule a mediation session within weeks or months, rather than waiting years for a trial date.
Confidentiality is another big plus. Unlike court proceedings, which are generally public, mediation discussions are private. This can be particularly appealing if you’re dealing with sensitive medical issues or if you’re worried about publicity affecting your personal or professional life.
Mediation also gives you more control over the outcome. In a trial, you’re at the mercy of the judge or jury. In mediation, you have a say in the final agreement. If you’re not happy with what’s being offered, you can walk away and continue with litigation.
There’s also the emotional factor to consider. Trials can be stressful and confrontational. Mediation, while still challenging, tends to be less adversarial. It can provide a space for you to express your concerns and feelings in a way that’s not always possible in a courtroom.
Finally, mediation can preserve relationships. If you need ongoing care from the same healthcare provider or institution, resolving your dispute through mediation might make it easier to maintain that relationship going forward.
Structured Settlements
When it comes to receiving your settlement, it’s not always a simple matter of getting a big check and calling it a day. Structured settlements have become increasingly common in medical malpractice cases, especially those involving long-term injuries or disabilities.
In a structured settlement, instead of receiving a lump sum, you get payments spread out over time. These payments can be tailored to your specific needs. For example, you might get larger payments early on to cover immediate medical expenses, then smaller regular payments to help with ongoing care or lost wages.
One of the main advantages of structured settlements is financial security. They can provide a steady income stream, which can be particularly beneficial if you’re unable to work due to your injury. They also offer some protection against the risk of burning through a large lump sum too quickly.
Structured settlements can be complex, though. Once you agree to a structure, it’s usually difficult or impossible to change. That’s why it’s crucial to work with financial advisors and experienced attorneys to ensure the structure meets your long-term needs.
Tax Implications
The tax implications of medical malpractice settlements can be a bit of a minefield. Generally speaking, compensation for physical injuries or illness is not taxable under federal law. This includes both lump sum payments and structured settlements for medical expenses and pain and suffering related to physical injuries.
However, there are exceptions. If you deducted medical expenses related to your injury on past tax returns and then received compensation for those expenses in your settlement, you might need to report that as income. It’s a bit like a refund of those deductions.
Punitive damages, if awarded, are typically taxable. These are damages meant to punish the defendant rather than compensate you for your injuries. If your settlement includes punitive damages, it’s important to have them clearly separated from compensatory damages in the settlement agreement.
Interest on your settlement can also be taxable. If there’s a delay between when the settlement is agreed upon and when you receive the money, any interest accrued during that time is generally considered taxable income.
Structured settlements can offer some tax advantages. The full amount of the settlement is tax-free at the time of the agreement, even if it’s paid out over many years. This can be a significant benefit compared to taking a lump sum and investing it yourself, where you might have to pay taxes on the investment gains.
Given the complexity of tax law and the high stakes involved in medical malpractice settlements, it’s crucial to work with tax professionals who have experience in this area. They can help you structure your settlement in the most tax-efficient way possible and ensure you’re complying with all relevant tax laws.
Medical Malpractice Settlement Trends in 2024
The landscape of medical malpractice settlements is always evolving, and 2024 is no exception. We’re seeing some interesting trends that could impact how these cases play out.
One major trend is the increasing use of technology in both healthcare and the legal process. Telemedicine has exploded in popularity, bringing with it new questions about standards of care and liability. At the same time, artificial intelligence and big data are being used more frequently in case evaluation and settlement negotiations.
We’re also seeing a shift in how juries perceive medical malpractice cases. The COVID-19 pandemic has put healthcare workers in the spotlight, often casting them as heroes. This could potentially make juries more sympathetic to healthcare providers in malpractice cases.
On the flip side, there’s growing awareness of systemic issues in healthcare, like racial disparities in treatment outcomes. This could lead to more scrutiny of healthcare practices and potentially larger settlements in cases where these issues play a role.
Average Settlement Amounts
When it comes to average settlement amounts, it’s important to remember that every case is unique. That said, looking at averages can give us a general sense of the landscape.
In 2024, we’re seeing some interesting patterns emerge. Overall, average settlement amounts have been trending upward. This isn’t just due to inflation—there’s been a real increase in the value placed on certain types of injuries and damages.
Brain injuries continue to command some of the highest settlements, often reaching into the millions. This reflects the devastating long-term impact these injuries can have on a person’s life. Spinal cord injuries and birth injuries also tend to result in higher-than-
Brain injuries continue to command some of the highest settlements, often reaching into the millions. This reflects the devastating long-term impact these injuries can have on a person’s life. Spinal cord injuries and birth injuries also tend to result in higher-than-average settlements.
We’re also seeing a trend towards higher settlements in cases involving missed or delayed cancer diagnoses. As cancer treatments continue to advance, the argument that early detection could have made a significant difference in outcomes is becoming more compelling.
It’s worth noting that these averages can vary widely by state and even by county. Some jurisdictions are known for higher settlements, while others tend to be more conservative. Your location can have a big impact on what’s considered an “average” settlement.
Factors Affecting Averages
While averages can be useful benchmarks, it’s crucial to understand the factors that can push settlements above or below these figures. One major factor is the reputation and track record of the healthcare provider or institution involved. High-profile hospitals or doctors might be more inclined to settle quickly and generously to avoid negative publicity.
The specific circumstances of the alleged malpractice also play a huge role. Cases involving clear-cut errors, like operating on the wrong body part, tend to settle for higher amounts than more complex cases where the standard of care is less clear-cut.
The age of the patient is another significant factor. Cases involving young victims, especially children, often result in higher settlements due to the long-term impact on their lives and potential earnings.
The economic damages involved—things like medical bills and lost wages—can vary widely depending on the patient’s circumstances. A high-earning professional who can no longer work due to malpractice might see a much higher settlement than someone with lower earning potential.
Finally, the skill and experience of the legal teams on both sides can significantly impact settlement amounts. A savvy attorney who knows how to build a compelling case and negotiate effectively can often secure higher settlements.
Impact of COVID-19 on Settlements
The COVID-19 pandemic has left an indelible mark on the healthcare system, and its effects are still rippling through medical malpractice settlements in 2024. We’ve seen a shift in the types of cases being filed, with more claims related to delayed diagnoses or treatment due to pandemic-related healthcare disruptions.
There’s also been a notable impact on jury perceptions. The public’s increased awareness of the challenges faced by healthcare workers during the pandemic has, in some cases, led to more sympathetic juries. This could potentially result in lower settlement offers from defendants who feel more confident about their chances at trial.
On the flip side, the pandemic has also highlighted systemic issues in healthcare, particularly regarding preparedness for public health crises. This increased scrutiny could lead to higher settlements in cases where systemic failures played a role in patient harm.
Telehealth Malpractice Considerations
The boom in telehealth services has opened up new frontiers in medical malpractice law. Virtual consultations bring unique challenges when it comes to determining liability and appropriate care standards.
One key issue is the limitations of remote examinations. Without the ability to physically examine a patient, doctors may miss crucial signs or symptoms. This has led to an increase in claims related to misdiagnosis or delayed diagnosis in telehealth settings.
There’s also the question of technology failures. What happens if a poor internet connection leads to miscommunication or a missed symptom? These cases are pushing courts to redefine what constitutes a reasonable standard of care in virtual healthcare settings.
Privacy and data security are other hot-button issues in telehealth malpractice. Breaches of patient confidentiality or unauthorized access to virtual appointments could potentially lead to new types of malpractice claims.
As telehealth continues to evolve, we’re likely to see more precedent-setting cases that help define the boundaries of malpractice in virtual healthcare settings.
Caps on Damages
Damage caps remain a contentious issue in medical malpractice law, and the landscape continues to shift in 2024. These caps, which limit the amount of compensation a plaintiff can receive, particularly for non-economic damages like pain and suffering, vary widely from state to state.
Some states have maintained strict caps, arguing that they help keep malpractice insurance costs down and prevent doctors from practicing “defensive medicine.” Others have loosened or eliminated their caps, often in response to legal challenges or changing public sentiment.
In states with caps, we’re seeing more creative legal strategies to maximize compensation within the limits. This might involve focusing more on economic damages, which are often not subject to caps, or pursuing claims against multiple defendants to increase the overall potential recovery.
It’s worth noting that these caps can significantly impact settlement negotiations. In states with low caps, defendants might be less inclined to offer high settlements, knowing their potential liability at trial is limited.
Constitutional Challenges
The constitutionality of damage caps remains a hot topic in 2024. Several states have seen their caps challenged on various grounds, including equal protection and the right to a jury trial.
Some state supreme courts have struck down damage caps as unconstitutional. These decisions often argue that caps arbitrarily limit compensation for the most severely injured patients, violating principles of equal protection under the law.
Other courts have upheld caps, viewing them as a legitimate exercise of legislative power to address issues in the healthcare system. These rulings often cite concerns about the availability and affordability of medical care as justification for the caps.
These ongoing legal battles create a dynamic landscape for medical malpractice settlements. A successful constitutional challenge in one state can have ripple effects, influencing similar challenges in other jurisdictions or even prompting legislative changes.
For plaintiffs and their attorneys, staying informed about these constitutional challenges is crucial. A cap that’s in place when a case is filed might be struck down by the time it reaches settlement negotiations or trial, potentially dramatically altering the value of the case.
Maximum Payouts and Outlier Cases
While average settlements provide a general picture, it’s the exceptional cases that often grab headlines and push the boundaries of what’s possible in medical malpractice compensation. These outlier cases, with their eye-popping payouts, can have a significant impact on the broader landscape of malpractice settlements.
Factors that contribute to these maximum payouts often include catastrophic injuries, clear-cut negligence, sympathetic plaintiffs, and skilled legal representation. Cases involving permanent disability, especially in young patients with long life expectancies, can result in settlements or verdicts in the tens of millions of dollars.
It’s important to note that these extreme cases are rare and shouldn’t be seen as typical. However, they can influence settlement negotiations in other cases by setting new benchmarks for what’s possible in certain types of claims.
Record-Breaking Settlements
Every so often, a medical malpractice case results in a settlement that shatters previous records. These landmark cases often involve devastating injuries or particularly egregious negligence.
One recent record-breaker involved a birth injury case that resulted in severe brain damage to the child. The settlement, which exceeded $200 million, took into account the lifetime of care the child would require and the impact on the family.
Another notable case involved a missed diagnosis that led to a patient becoming quadriplegic. The settlement, which approached $100 million, factored in the patient’s young age and the dramatic change in their quality of life.
It’s worth noting that these massive settlements often involve structured payouts over many years, rather than lump sums. They may also include provisions for ongoing medical care or life care plans.
While these record-breaking cases are outliers, they serve an important purpose in the legal system. They can act as deterrents, encouraging healthcare providers and institutions to maintain high standards of care. They also help establish precedents that can benefit other patients who have suffered similar injuries.
Catastrophic Injury Cases
Catastrophic injury cases often result in the highest settlements in medical malpractice law. These cases involve injuries that have life-altering, long-term consequences for the patient.
Brain injuries are frequently at the top of this list. The complex nature of the brain means that injuries can have wide-ranging effects on cognitive function, personality, and physical abilities. Settlements in these cases need to account for a lifetime of care and support.
Spinal cord injuries, particularly those resulting in paralysis, also tend to see very high settlements. These cases often involve not just medical care, but also modifications to homes and vehicles, ongoing physical therapy, and compensation for lost earning capacity.
Birth injuries that result in conditions like cerebral palsy can lead to substantial settlements. These cases are particularly poignant as they involve injuries that will affect the entire course of a child’s life.
In catastrophic injury cases, the settlement often needs to cover not just past and current medical expenses, but also future care needs. This might include round-the-clock nursing care, specialized equipment, and repeated surgeries or treatments over the course of the patient’s lifetime.
The emotional toll of catastrophic injuries is also a significant factor in these settlements. Compensation for pain and suffering, loss of enjoyment of life, and emotional distress can make up a large portion of the settlement in these severe cases.
Wrongful Death Settlements
Wrongful death cases in medical malpractice represent some of the most emotionally charged and complex claims. These cases arise when a patient dies as a result of medical negligence, and the family seeks compensation for their loss.
Settlements in wrongful death cases can vary widely depending on the circumstances. Factors that can influence the settlement amount include the age and earning potential of the deceased, the nature of the medical error, and the state’s specific laws regarding wrongful death claims.
One unique aspect of wrongful death settlements is that they often need to balance competing interests within the family. Different family members may have different priorities or ideas about what constitutes fair compensation. This can add an extra layer of complexity to settlement negotiations.
It’s worth noting that some states place caps on wrongful death damages, which can limit the potential payout in these cases. However, these caps are often subject to legal challenges, and the landscape continues to evolve.
Survivor Benefits
In wrongful death cases, the focus shifts to compensating the surviving family members. These survivor benefits aim to address both the financial and emotional toll of losing a loved one to medical malpractice.
Economic damages in these cases often include compensation for lost financial support. This might cover the deceased’s expected lifetime earnings, benefits like health insurance or pension plans, and even the value of services they provided to the family (like childcare or home maintenance).
Non-economic damages can be substantial in wrongful death cases. These might include compensation for loss of companionship, guidance, and emotional support. In cases involving the death of a child, parents might be compensated for the loss of the joy and comfort that the child would have provided throughout their life.
Some states allow for punitive damages in particularly egregious cases of medical negligence leading to death. These damages are intended to punish the wrongdoer and deter similar conduct in the future.
It’s important to note that laws regarding survivor benefits vary significantly from state to state. Some states limit who can file a wrongful death claim or receive benefits, while others have more inclusive laws. Understanding these state-specific rules is crucial for families pursuing wrongful death claims.
Learnings Recap
We’ve covered a lot of ground in our exploration of medical malpractice settlements in 2024. From the basics of proving negligence to the complexities of negotiating settlements and understanding current trends, you’re now equipped with a comprehensive overview of this challenging legal landscape.
Key takeaways include:
- The four elements of medical negligence: duty, breach, causation, and damages
- The critical importance of timely action due to statutes of limitations
- The role of strong evidence, including expert testimonies, in building a compelling case
- Factors influencing settlements, such as injury severity, evidence quality, and jurisdiction tendencies
- The potential benefits of alternative dispute resolution methods like mediation
- The pros and cons of structured settlements and their tax implications
- Current trends shaping the medical malpractice landscape, including the impact of COVID-19 and the rise of telehealth
- The ongoing debate over damage caps and their constitutional challenges
- The unique considerations in catastrophic injury and wrongful death cases
Discover how our comprehensive approach to injury cases applies to medical malpractice settlements.




