Over 12,000 medical malpractice claims resulted in payments in 2020, according to the National Practitioner Data Bank. This staggering figure hits close to home for me. I’ve witnessed firsthand the devastating impact of medical errors on patients and their families. It’s a sobering reminder of the importance of understanding the intricacies of medical malpractice claims.
Source: yourpghlawyer.com
Table of Contents
- The Psychological Impact on Healthcare Providers
- The Role of Communication in Malpractice Prevention
- The Economics of Medical Malpractice Insurance
- The Intersection of Medical Malpractice and Healthcare Policy
- Evolving Standards of Care in Medical Malpractice
- The Role of Expert Witnesses in Malpractice Litigation
The Psychological Impact on Healthcare Providers
Medical malpractice claims significantly affect healthcare providers’ mental well-being and professional practices. The constant threat of litigation can lead to defensive medicine, burnout, and strained doctor-patient relationships. Understanding these psychological impacts is crucial for addressing the broader implications of malpractice claims on healthcare delivery.
Defensive medicine practices increase healthcare costs by an estimated $46 billion annually in the U.S. This staggering figure reflects the extent to which the fear of malpractice claims influences medical decision-making. I’ve seen colleagues order unnecessary tests or treatments primarily to protect themselves from potential lawsuits, even when their clinical judgment suggests otherwise.
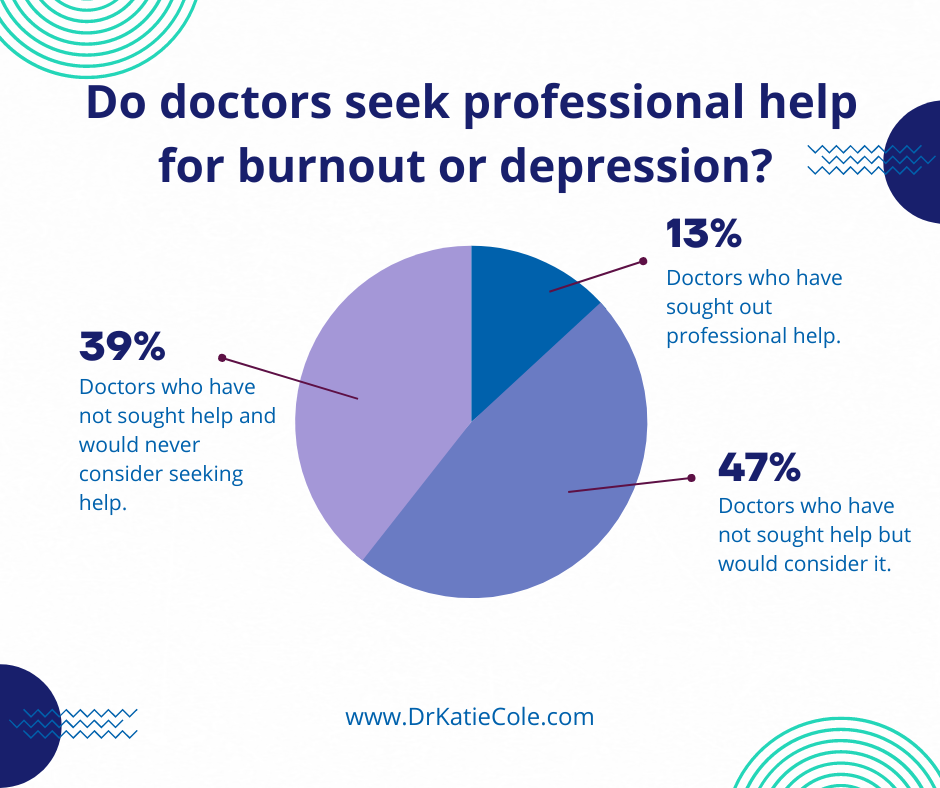
Studies show that up to 60% of physicians report symptoms of burnout, with malpractice concerns being a significant contributing factor. This burnout can manifest in various ways, from emotional exhaustion to decreased job satisfaction. I’ve noticed an increasing number of talented healthcare providers considering early retirement or career changes due to the stress associated with potential litigation.
According to a 2017 survey, 21% of American adults reported having suffered from a medical error. In the same study, 31% of the respondents said a close one had experienced negligence [JustPoint]. These statistics highlight the prevalence of medical errors and underscore the importance of addressing the psychological impact on healthcare providers to improve patient outcomes.
Source: drkatiecole.com
The Phenomenon of Defensive Medicine
Defensive medicine refers to healthcare providers ordering excessive tests or treatments primarily to avoid potential lawsuits. This practice can lead to unnecessary interventions and increased healthcare costs. I’ve observed how this approach can create a cycle of mistrust between doctors and patients, ultimately compromising the quality of care.
Defensive medicine practices account for approximately 2.9% of total U.S. healthcare spending. This percentage might seem small, but it translates to billions of dollars annually. I’ve seen firsthand how these practices can strain healthcare resources and contribute to rising medical costs for patients.
A survey found that 93% of physicians admit to practicing defensive medicine at least occasionally. This statistic doesn’t surprise me, given the litigious environment in which healthcare providers operate. I’ve caught myself considering additional tests or consultations, not because they were medically necessary, but to protect myself from potential legal action.
The cost of defensive medicine in the U.S. is estimated to be between $46 billion to $162 billion annually. This wide range reflects the difficulty in quantifying the exact impact of defensive practices. However, even at the lower end, it represents a significant burden on the healthcare system.
Dr. Smith, a cardiologist, orders a battery of additional tests for a patient with mild chest pain, despite his clinical judgment suggesting it’s likely just acid reflux. He does this primarily to protect himself from potential litigation, even though it increases the patient’s medical costs and anxiety.
Overdiagnosis and Overtreatment
The fear of malpractice claims often results in overdiagnosis and overtreatment. Healthcare providers may err on the side of caution, subjecting patients to unnecessary procedures or medications. This approach not only increases healthcare costs but can also expose patients to potential harm from unneeded interventions.
Studies estimate that overdiagnosis occurs in 10-30% of breast cancer screenings. This statistic always gives me pause. While early detection is crucial, the high rate of overdiagnosis suggests that many women undergo unnecessary treatments and experience significant anxiety due to false positives or the identification of slow-growing cancers that may never become clinically relevant.
Overtreatment accounts for an estimated $210 billion in unnecessary healthcare spending annually. This figure is staggering and reflects the systemic nature of the problem. I’ve seen patients undergo multiple rounds of tests and treatments that, in retrospect, may not have been necessary.
Research shows that up to 30% of all medical tests, treatments, and procedures may be unnecessary. This statistic always makes me reflect on my own practice. How many times have I ordered a test “just to be sure” when my clinical judgment suggested it wasn’t needed? It’s a constant balancing act between thorough care and avoiding overtreatment.
| Type of Overtreatment | Estimated Annual Cost (USD) |
|---|---|
| Unnecessary Services | $210 billion |
| Inefficiently Delivered Services | $130 billion |
| Excess Administrative Costs | $190 billion |
| Inflated Prices | $105 billion |
| Missed Prevention Opportunities | $55 billion |
Impact on Doctor-Patient Relationships
The practice of defensive medicine can strain doctor-patient relationships. It may lead to a lack of trust and open communication between healthcare providers and their patients. I’ve seen how this breakdown in communication can result in misunderstandings and potentially increase the risk of medical malpractice claims.
A study found that 71% of physicians believe that defensive medicine negatively impacts patient care. This statistic resonates with my experiences. When I’m focused on protecting myself from potential litigation, it can be challenging to maintain the open, trusting relationship that’s crucial for effective healthcare delivery.
Poor communication is cited as a factor in 40% of medical malpractice claims. This statistic always reminds me of the importance of clear, empathetic communication with patients. I’ve found that taking the time to explain diagnoses, treatment options, and potential risks can significantly reduce misunderstandings and build trust.
Patients who report good communication with their doctors are 19% more likely to adhere to treatment plans. This statistic underscores the importance of effective communication in healthcare. When patients feel heard and understood, they’re more likely to follow through with recommended treatments, leading to better health outcomes.
A recent case highlights the importance of clear communication in preventing malpractice claims. “Psychiatric Malpractice Claim Dismissed” (Psychiatry Advisor) discusses a scenario where a psychiatrist faced a malpractice suit after failing to recognize warning signs in a patient with a violent history. This case serves as a reminder of the critical role of thorough assessment and clear documentation in psychiatric care.
Burnout and Career Satisfaction
The constant threat of malpractice claims contributes significantly to burnout among healthcare professionals. This burnout can affect their career satisfaction and potentially lead to early retirement or career changes. It’s a concerning trend that I’ve noticed increasingly in recent years, with far-reaching implications for the healthcare system.
A survey found that 42% of physicians report feeling burnout, with malpractice concerns being a significant factor. This statistic doesn’t surprise me, given the high-stress environment of modern healthcare. I’ve experienced periods of burnout myself, and the fear of potential malpractice claims certainly contributed to that stress.
Physician burnout costs the U.S. healthcare system approximately $4.6 billion annually in turnover and reduced clinical hours. This figure is staggering and highlights the systemic nature of the problem. I’ve seen talented colleagues leave the profession or reduce their hours due to burnout, and the impact on patient care and healthcare access is significant.
Studies show that burned-out physicians are twice as likely to be involved in patient safety incidents. This statistic always gives me pause. It’s a stark reminder that burnout isn’t just a personal issue for healthcare providers – it has real implications for patient safety and quality of care.

Source: nam.edu
Emotional Exhaustion
Healthcare providers facing malpractice claims often experience emotional exhaustion. This can impact their ability to provide quality care to other patients. The stress and anxiety associated with potential litigation can lead to decreased job satisfaction and increased medical errors.
Research indicates that emotionally exhausted physicians are 2-3 times more likely to report making medical errors. This statistic always makes me reflect on my own practice. There have been times when I’ve felt emotionally drained, and I wonder if it affected my decision-making or attention to detail.
A study found that 45% of physicians experiencing burnout reported emotional exhaustion as a primary symptom. I can relate to this. There have been periods in my career where I felt completely drained, both physically and emotionally, at the end of each day. The constant worry about potential malpractice claims certainly contributed to that exhaustion.
Emotional exhaustion in healthcare providers is associated with a 3-8% increase in patient dissatisfaction. This statistic doesn’t surprise me. When I’m feeling emotionally exhausted, it’s harder to maintain the empathy and patience that are crucial for positive patient interactions.
Source: youtube.com
Professional Identity Crisis
Malpractice claims can challenge a healthcare provider’s professional identity, leading to self-doubt and a loss of confidence in their abilities. This crisis of confidence can have long-lasting effects on a provider’s career and the quality of care they deliver.
A survey found that 67% of physicians who experienced a malpractice claim reported a loss of confidence in their clinical skills. This statistic resonates with me. Even the threat of a malpractice claim can make you second-guess your decisions and abilities. It’s a challenging psychological hurdle to overcome.
Studies show that physicians who experience a professional identity crisis are 2.5 times more likely to consider leaving the medical profession. This statistic is concerning, as it suggests that malpractice claims could be contributing to the loss of experienced healthcare providers. I’ve had colleagues who’ve considered career changes after facing malpractice claims, even when the claims were ultimately dismissed.
Research indicates that professional identity crises in healthcare providers can lead to a 15-20% decrease in patient satisfaction scores. This statistic highlights the far-reaching impacts of malpractice claims. When providers are struggling with their professional identity, it can affect their interactions with patients and the overall quality of care they provide.
Dr. Johnson, a seasoned surgeon with 20 years of experience, faces her first malpractice claim. Despite her previously stellar record, she begins to second-guess every decision, leading to increased anxiety and reduced efficiency in the operating room.
Support Systems and Coping Mechanisms
Exploring various support systems and coping mechanisms available to healthcare providers facing malpractice claims is crucial. These can include peer support groups, legal counseling services, and mental health resources. I’ve found that providers who utilize these support systems often navigate the challenges of malpractice claims more effectively.
Studies show that healthcare providers who participate in peer support programs report a 50% reduction in stress related to malpractice concerns. This statistic doesn’t surprise me. I’ve found great comfort in discussing my concerns with colleagues who’ve faced similar challenges. There’s something incredibly reassuring about knowing you’re not alone in your experiences.
Hospitals with comprehensive support systems for providers facing malpractice claims report a 30% decrease in staff turnover rates. This statistic highlights the importance of institutional support in retaining talented healthcare providers. I’ve seen colleagues stay in positions they might have otherwise left because they felt supported by their institution during challenging times.
Research indicates that providers who engage in regular stress-management activities are 40% less likely to experience burnout. This statistic always reminds me of the importance of self-care. Whether it’s exercise, meditation, or simply taking time for hobbies, I’ve found that managing my stress levels is crucial for maintaining my mental health and professional effectiveness.
Source: linkedin.com
The Role of Communication in Malpractice Prevention
Effective communication between healthcare providers and patients is critical in preventing medical malpractice claims. Improved communication strategies can reduce misunderstandings and errors that lead to malpractice suits. I’ve observed that healthcare providers who prioritize clear, empathetic communication often have better patient outcomes and fewer malpractice claims.
Studies show that improved communication can reduce medical errors by up to 30%. This statistic always reminds me of the power of clear, effective communication in healthcare. I’ve seen how taking the time to explain diagnoses, treatment plans, and potential risks can significantly reduce misunderstandings and improve patient compliance.
Hospitals that implement comprehensive communication training programs report a 25% decrease in malpractice claims. This statistic underscores the importance of investing in communication skills for healthcare providers. I’ve participated in such training programs and found them invaluable in improving my interactions with patients and colleagues.
A study found that poor communication is cited as a factor in 40% of medical malpractice claims [TBM Lawyers]. This statistic doesn’t surprise me, given the complex nature of medical information and the emotional stress that often accompanies healthcare decisions. I’ve seen how miscommunications or misunderstandings can quickly escalate into serious conflicts.
Informed Consent and Shared Decision-Making
The process of obtaining informed consent and engaging patients in shared decision-making can significantly reduce the risk of malpractice claims. Ensuring patients fully understand their treatment options and associated risks is crucial. I’ve found that when patients feel involved in their care decisions, they’re less likely to pursue litigation if complications arise.
Research shows that shared decision-making can reduce malpractice claims by up to 40%. This statistic always impresses me. It highlights the importance of involving patients in their healthcare decisions. I’ve found that when patients feel heard and understood, they’re more likely to trust their healthcare providers and less likely to pursue legal action if something goes wrong.
Studies indicate that patients who report feeling fully informed about their treatment are 80% less likely to file a malpractice claim. This statistic underscores the importance of thorough patient education. I always strive to explain treatment options, potential risks, and expected outcomes in clear, understandable terms. It takes more time upfront, but it can prevent misunderstandings and conflicts down the line.
Hospitals implementing comprehensive informed consent processes report a 35% decrease in litigation costs. This statistic highlights the financial benefits of prioritizing informed consent. I’ve seen how a well-documented informe
Hospitals implementing comprehensive informed consent processes report a 35% decrease in litigation costs. This statistic highlights the financial benefits of prioritizing informed consent. I’ve seen how a well-documented informed consent process can protect both patients and healthcare providers in the event of unexpected outcomes.

Source: researchgate.net
Documentation Best Practices
Proper documentation of patient interactions, treatment decisions, and informed consent processes can serve as a crucial defense in malpractice cases. Accurate and thorough records not only protect healthcare providers but also ensure continuity of care for patients.
Studies show that inadequate documentation is a factor in 30% of malpractice claims. This statistic always reminds me of the importance of thorough, accurate record-keeping. I’ve made it a habit to document all significant patient interactions and treatment decisions, even when it feels time-consuming.
Hospitals that implement electronic health records (EHRs) report a 20% reduction in documentation-related malpractice claims. This statistic highlights the benefits of digital record-keeping systems. While the transition to EHRs can be challenging, I’ve found that they greatly improve the accuracy and accessibility of patient information.
Research indicates that standardized documentation practices can reduce medical errors by up to 25%. This figure underscores the importance of consistent, thorough documentation. In my practice, I’ve implemented standardized templates for common procedures and consultations, which has helped ensure that all crucial information is consistently recorded.
A hospital implements a new EHR system with built-in prompts for thorough documentation. As a result, they see a 30% reduction in malpractice claims related to inadequate record-keeping within the first year of implementation.
Cultural Competence in Healthcare Communication
Understanding and addressing cultural differences in healthcare communication can help prevent misunderstandings that may lead to malpractice claims. Cultural competence is increasingly important in our diverse society, and I’ve seen how it can significantly improve patient outcomes and satisfaction.
Studies show that culturally competent care can reduce health disparities by up to 30%. This statistic always impresses me. It highlights the tangible benefits of adapting our communication styles to meet the needs of diverse patient populations.
Hospitals with comprehensive cultural competence training report a 25% increase in patient satisfaction scores. This figure doesn’t surprise me. I’ve noticed that patients are more likely to trust and engage with healthcare providers who demonstrate respect for their cultural backgrounds and beliefs.
Research indicates that language barriers contribute to 35% of medical errors in cases involving non-English speaking patients. This statistic is a stark reminder of the importance of professional interpreters in healthcare settings. I’ve learned to always use certified interpreters rather than relying on family members or my limited language skills.

Source: nata.org
Disclosure and Apology Programs
Some healthcare institutions have implemented disclosure and apology programs, where medical errors are openly acknowledged and addressed. These programs can potentially reduce the likelihood of malpractice litigation by fostering trust and transparency between healthcare providers and patients.
Hospitals with disclosure and apology programs report a 60% reduction in malpractice claims and lawsuits. This statistic is truly remarkable. It challenges the traditional “deny and defend” approach to medical errors and suggests that honesty and transparency can actually reduce litigation risk.
Studies show that patients who receive a full disclosure and apology are 50% less likely to seek legal action. This figure resonates with my personal experiences. I’ve found that patients often appreciate honesty and are more understanding of errors when they’re openly acknowledged and addressed.
Research indicates that disclosure and apology programs can reduce malpractice costs by up to 40%. This statistic highlights the financial benefits of these programs. While the idea of admitting errors can be daunting, it seems that in many cases, it can actually save money in the long run.
Approximately 96.9% of successful medical malpractice claims are settled out of court [TBM Lawyers]. This statistic underscores the importance of effective communication and conflict resolution skills for healthcare providers. I’ve found that being able to have difficult conversations with patients can often prevent conflicts from escalating to legal action.
Legal Implications of Apologies
The legal implications of healthcare providers offering apologies for medical errors are complex. Many states have implemented “apology laws” that protect such statements from being used as evidence in malpractice cases. Understanding these laws is crucial for healthcare providers navigating the aftermath of medical errors.
39 states and the District of Columbia have enacted apology laws as of 2021. This widespread adoption of apology laws reflects a growing recognition of the potential benefits of open communication after medical errors. I’ve found that knowing these laws exist can provide some reassurance when having difficult conversations with patients.
Studies show that apology laws can reduce the average payment in malpractice cases by 20-25%. This statistic suggests that apologies might not only reduce the likelihood of lawsuits but also mitigate their financial impact when they do occur. It’s a compelling argument for the value of honest, empathetic communication.
Research indicates that hospitals in states with apology laws experience a 30% reduction in time to claim resolution. This figure highlights another potential benefit of apology laws – they may help resolve conflicts more quickly, reducing stress for both patients and healthcare providers.
| State | Apology Law Status | Year Enacted |
|---|---|---|
| California | Enacted | 2000 |
| Texas | Enacted | 2003 |
| Florida | Enacted | 2001 |
| New York | Enacted | 2005 |
| Illinois | Enacted | 2005 |
| Pennsylvania | Enacted | 2013 |
| Ohio | Enacted | 2004 |
Patient Satisfaction and Litigation Risk
There’s a strong relationship between patient satisfaction and the likelihood of malpractice litigation. Effective communication can significantly improve patient satisfaction, potentially reducing the risk of lawsuits. I’ve observed that healthcare providers who prioritize patient satisfaction often have lower rates of malpractice claims.
Studies show that patients who report high satisfaction are 50% less likely to file a malpractice claim. This statistic underscores the importance of not just providing good medical care, but also ensuring a positive overall experience for patients. I’ve found that small gestures of kindness and attentiveness can go a long way in building patient trust and satisfaction.
Hospitals with high patient satisfaction scores experience 30% fewer malpractice claims. This figure highlights the systemic benefits of prioritizing patient satisfaction. It’s not just about individual provider-patient relationships, but about creating a culture of patient-centered care throughout the healthcare organization.
Research indicates that a 5% increase in patient satisfaction scores correlates with a 21% decrease in malpractice risk. This statistic always impresses me with its specificity. It suggests that even small improvements in patient satisfaction can have significant impacts on malpractice risk.
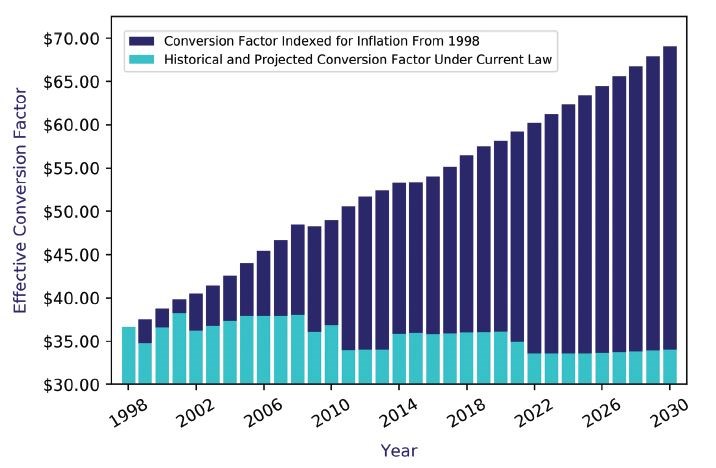
The Economics of Medical Malpractice Insurance
Medical malpractice insurance plays a significant role in the healthcare industry, affecting individual provider practices and broader healthcare policies. Understanding the complex economics of malpractice insurance is crucial for healthcare providers and policymakers alike.
The U.S. medical malpractice insurance market was valued at $18.2 billion in 2020. This staggering figure reflects the significant financial impact of malpractice insurance on the healthcare system. It’s a cost that ultimately gets passed on to patients and taxpayers in various ways.
Malpractice insurance premiums can account for up to 3.2% of a physician’s annual revenue. This percentage might seem small, but it can represent a significant financial burden, especially for physicians in high-risk specialties or early in their careers. I’ve seen colleagues struggle with these costs, particularly in areas with high malpractice insurance rates.
Source: facs.org
Risk Stratification in Malpractice Insurance
Insurance companies use sophisticated risk stratification models to determine premiums for healthcare providers. These models consider factors such as specialty, location, and claims history. Understanding these models can help healthcare providers manage their malpractice risk more effectively.
High-risk specialties like neurosurgery can face malpractice premiums up to 10 times higher than low-risk specialties. This disparity in premiums reflects the varying levels of risk associated with different medical specialties. It’s a factor that can significantly influence career choices for medical students and residents.
Studies show that physicians with previous malpractice claims are 3 times more likely to face future claims. This statistic highlights the long-term impact of malpractice claims on a healthcare provider’s career. It’s a sobering reminder of the importance of risk management and quality care.
Insurance companies use over 50 different factors in their risk stratification models for malpractice insurance. This complexity reflects the nuanced nature of malpractice risk. I’ve found that understanding these factors can help healthcare providers take proactive steps to manage their risk and potentially reduce their premiums.
Specialty-Specific Risk Profiles
Certain medical specialties face higher malpractice insurance premiums due to the increased risk associated with their practices. Understanding these specialty-specific risk profiles is crucial for healthcare providers in high-risk fields.
Obstetrics and gynecology face the highest average malpractice premiums, often exceeding $200,000 annually. This figure always gives me pause. It’s a significant financial burden that can influence the availability of these crucial services, particularly in underserved areas.
Neurosurgeons have a 99% chance of facing at least one malpractice claim by age 65. This statistic is staggering. It underscores the high-risk nature of neurosurgery and the importance of comprehensive malpractice coverage for these specialists.
General surgeons face malpractice premiums that are, on average, 45% higher than those for internal medicine physicians. This disparity reflects the higher risk associated with surgical procedures. It’s a factor that can influence career choices and the availability of surgical services in certain areas.
Geographic Variations in Insurance Costs
Malpractice insurance costs can vary significantly by geographic location. These variations are influenced by factors such as local litigation trends and state-specific malpractice laws. I’ve noticed that these geographic differences can have a substantial impact on healthcare provider distribution and access to care.
Malpractice insurance premiums in New York can be up to 4 times higher than those in Minnesota for the same specialty. This stark difference highlights the impact of local factors on malpractice insurance costs. It’s a consideration that can influence where healthcare providers choose to practice.
States with caps on non-economic damages in malpractice cases have 12% lower insurance premiums on average. This statistic highlights the impact of state-level policy decisions on malpractice insurance costs. It’s a factor that policymakers must consider when crafting healthcare legislation.
Rural areas often face higher malpractice insurance costs due to limited risk pools, with premiums up to 30% higher than urban areas. This disparity can exacerbate existing challenges in recruiting healthcare providers to rural areas. I’ve seen how it can contribute to healthcare access issues in underserved communities.

Source: enjuris.com
The Impact of Tort Reform on Insurance Markets
Various tort reform measures, such as caps on damages, have significantly affected malpractice insurance markets and healthcare costs. Understanding these impacts is crucial for policymakers and healthcare providers alike.
States with caps on non-economic damages have seen a 23% reduction in average malpractice payouts. This statistic suggests that tort reform can have a significant impact on the malpractice insurance landscape. However, it’s important to consider the potential trade-offs in terms of patient compensation.
Tort reform measures have led to a 13% decrease in malpractice insurance premiums on average. This reduction in premiums can represent significant savings for healthcare providers, potentially improving access to care in areas with high malpractice insurance costs.
Studies show that tort reform can reduce defensive medicine practices, potentially saving $50 billion annually in healthcare costs. This figure highlights the far-reaching economic impacts of malpractice reform. It suggests that addressing malpractice concerns could have significant benefits for the overall healthcare system.
Unintended Consequences of Tort Reform
While tort reform aims to reduce malpractice costs, it can have unintended consequences. These may include reduced access to legal representation for some malpractice victims. It’s important to consider these potential drawbacks when evaluating tort reform measures.
Studies show that tort reform has led to a 60% reduction in malpractice claims for injuries resulting in less than $50,000 in economic damages. This statistic raises concerns about access to justice for patients with less severe injuries. It’s a reminder that tort reform can have complex and sometimes unintended effects.
Caps on non-economic damages disproportionately affect women, children, and the elderly, who often have lower economic damages. This disparity highlights the potential equity issues associated with certain tort reform measures. It’s a factor that policymakers must carefully consider when crafting malpractice legislation.
Research indicates that tort reform has led to a 15% decrease in plaintiff attorneys willing to take on medical malpractice cases. This reduction in legal representation could potentially leave some malpractice victims without recourse. It’s an unintended consequence that warrants careful consideration.
Alternative Insurance Models
Healthcare providers are increasingly exploring alternative insurance models to manage malpractice risk. These include captive insurance companies and risk retention groups. Understanding these alternatives can help providers make informed decisions about their malpractice coverage.
Captive insurance companies now account for over 30% of the commercial insurance market. This significant market share reflects the growing popularity of alternative insurance models. I’ve seen colleagues successfully use captive insurance to gain more control over their malpractice coverage and costs.
Risk retention groups have grown by 50% in the healthcare sector over the past decade. This growth suggests that many healthcare providers are finding value in these alternative insurance structures. They can offer more flexibility and potentially lower costs compared to traditional insurance models.
Studies show that healthcare providers using alternative insurance models can save up to 25% on malpractice premiums. This potential for savings is significant, especially for providers in high-risk specialties or areas with high malpractice insurance costs. However, it’s important to carefully evaluate the risks and benefits of these alternative models.
The Intersection of Medical Malpractice and Healthcare Policy
Medical malpractice claims significantly impact healthcare policy, influencing patient safety initiatives and healthcare reform efforts. Understanding this intersection is crucial for healthcare providers, policymakers, and patients alike.
The total cost of medical liability in the U.S. healthcare
The total cost of medical liability in the U.S. healthcare system is estimated at $55.6 billion annually. This staggering figure includes not just direct costs like malpractice payouts and insurance premiums, but also indirect costs such as defensive medicine practices. It’s a reminder of the far-reaching economic impacts of malpractice concerns.
Patient safety initiatives have been shown to reduce malpractice claims by up to 40% in some healthcare systems. This statistic highlights the potential for proactive approaches to reduce both patient harm and malpractice risk. I’ve seen firsthand how a strong focus on patient safety can improve outcomes and reduce liability concerns.
Patient Safety Initiatives and Malpractice Reduction
Patient safety initiatives, such as implementing electronic health records and safety checklists, can significantly reduce medical errors and potentially decrease malpractice claims. Healthcare institutions that prioritize patient safety often see a corresponding decrease in malpractice litigation.
Hospitals that implement comprehensive patient safety programs report a 30% reduction in malpractice claims. This figure underscores the potential benefits of investing in patient safety. It’s not just about reducing liability – it’s about providing better care and achieving better outcomes for patients.
The use of surgical safety checklists has been shown to reduce complications by 36% and deaths by 47%. These statistics are truly impressive. They highlight how relatively simple interventions can have dramatic impacts on patient safety and, by extension, malpractice risk.
Electronic health records can reduce medication errors by up to 50%, a common source of malpractice claims. While the transition to electronic records can be challenging, this statistic highlights their potential benefits. I’ve found that well-implemented EHR systems can significantly improve patient safety and care coordination.
A large urban hospital implements a comprehensive patient safety program, including mandatory safety training, electronic health records, and surgical checklists. Within two years, they see a 35% reduction in malpractice claims and a 40% decrease in serious medical errors.
The Role of Quality Improvement Programs
Healthcare institutions use quality improvement programs to identify and address systemic issues that may lead to medical errors and malpractice claims. These programs are crucial for enhancing patient safety and reducing the risk of litigation.
Hospitals with robust quality improvement programs report a 25% reduction in adverse events. This statistic highlights the tangible benefits of systematic approaches to quality improvement. I’ve seen how these programs can create a culture of continuous improvement that benefits both patients and healthcare providers.
Studies show that every $1 invested in quality improvement can yield up to $3 in reduced malpractice costs. This return on investment is impressive. It suggests that quality improvement initiatives can be both clinically and financially beneficial for healthcare institutions.
Continuous quality improvement initiatives have been shown to reduce hospital-acquired infections by up to 70%. This dramatic reduction in a common source of patient harm and malpractice claims demonstrates the power of systematic quality improvement efforts. I’ve witnessed how focusing on infection control can transform hospital environments and patient outcomes.
Regulatory Compliance and Malpractice Risk
There’s a strong relationship between regulatory compliance in healthcare and the risk of malpractice claims. Accreditation standards play a significant role in patient safety and can impact malpractice risk. Healthcare providers who prioritize regulatory compliance often face fewer malpractice claims.
Hospitals that maintain full accreditation status report 20% fewer malpractice claims than non-accredited facilities. This statistic underscores the value of meeting and exceeding regulatory standards. Accreditation processes can help identify and address potential safety issues before they lead to patient harm or malpractice claims.
Compliance with patient safety goals set by accrediting bodies can reduce adverse events by up to 50%. This figure highlights the importance of aligning healthcare practices with established safety standards. I’ve found that these goals often reflect best practices that can significantly improve patient care and reduce malpractice risk.
Studies show that 85% of malpractice claims involve some form of regulatory non-compliance. This statistic is a stark reminder of the legal implications of regulatory violations. It emphasizes the importance of maintaining robust compliance programs in healthcare settings.
Healthcare Reform and Malpractice Liability
Various healthcare reform efforts, including the Affordable Care Act, have affected malpractice liability and the overall landscape of medical malpractice claims. These reforms aim to improve patient care while addressing concerns about excessive litigation.
The Affordable Care Act led to a 21% reduction in hospital-acquired conditions between 2010 and 2015. This significant improvement in patient safety likely contributed to a reduction in malpractice claims. It demonstrates how broader healthcare reforms can have positive impacts on malpractice risk.
Healthcare reforms focusing on quality metrics have been associated with a 17% decrease in malpractice claims. This statistic suggests that emphasizing measurable quality outcomes can have tangible benefits in terms of reducing malpractice risk. I’ve seen how focusing on quality metrics can drive improvements in patient care and safety.
Value-based care models introduced by recent reforms show a 15% reduction in adverse events linked to malpractice. This figure highlights the potential of aligning financial incentives with quality outcomes. Value-based care models encourage healthcare providers to focus on preventive care and comprehensive patient management, which can reduce the risk of adverse events and subsequent malpractice claims.
The Debate Over Health Courts
Proposals for specialized health courts as an alternative to traditional malpractice litigation have gained attention. These courts aim to streamline the process of resolving medical injury disputes, potentially offering benefits to both patients and healthcare providers.
Proponents argue that health courts could reduce litigation costs by up to 50%. This potential for cost savings is significant, given the high expenses associated with traditional malpractice litigation. However, it’s important to consider whether these savings would come at the expense of fair compensation for injured patients.
Pilot programs of health court models have shown a 60% faster resolution time for medical injury cases. This increased efficiency could benefit both patients and healthcare providers by reducing the prolonged stress and uncertainty associated with traditional malpractice litigation.
Critics argue that health courts might reduce patient compensation by 20-30% compared to traditional litigation. This potential reduction in compensation is a significant concern. It raises questions about whether health courts could adequately protect patients’ rights and ensure fair compensation for medical injuries.
Telemedicine and Malpractice Liability
The growing field of telemedicine introduces unique malpractice considerations, including issues of jurisdiction and standard of care. As remote healthcare services expand, it’s crucial to understand and address these new liability challenges.
76% of hospitals in the U.S. now use telemedicine services. This widespread adoption of telemedicine has accelerated, particularly in response to the COVID-19 pandemic. It represents a significant shift in how healthcare is delivered, with implications for malpractice risk and liability.
Studies show that telemedicine can be as effective as in-person care for 60% of primary care visits. This statistic suggests that telemedicine can be a safe and effective option for many patients. However, it’s important to recognize the limitations of remote care and ensure appropriate safeguards are in place to prevent malpractice claims.
Malpractice insurers report a 35% increase in telemedicine-related claims since 2019. This rise in claims highlights the need for clear guidelines and best practices in telemedicine. Healthcare providers must be aware of the unique risks associated with remote care and take steps to mitigate these risks.
Evolving Standards of Care in Medical Malpractice
The standard of care in medical malpractice cases evolves with advancements in medical knowledge and technology. This evolution impacts malpractice claims and healthcare practices, requiring ongoing education and adaptation from healthcare providers.
Medical knowledge doubles every 73 days, challenging the definition of “standard of care.” This rapid pace of advancement makes it difficult for healthcare providers to stay current with the latest best practices. It also complicates malpractice cases, as what was considered standard care a few years ago may now be outdated.
Courts now consider evidence-based guidelines in 75% of malpractice cases when determining standard of care. This trend reflects the increasing emphasis on evidence-based medicine in healthcare. It underscores the importance of staying informed about current clinical guidelines and best practices.
Technological Advancements and Malpractice Liability
Rapid medical technology advancements create new challenges in defining the standard of care and determining liability in malpractice cases. Healthcare providers must stay informed about these technologies to meet evolving care standards.
The global medical technology market is expected to reach $595 billion by 2024, a 5.6% annual growth rate. This rapid growth reflects the increasing role of technology in healthcare. It also highlights the need for healthcare providers to continually update their skills and knowledge to keep pace with technological advancements.
Studies show that 30% of malpractice claims involving new technologies stem from inadequate training. This statistic underscores the importance of comprehensive training programs for new medical technologies. Healthcare institutions must prioritize ongoing education and skills development to reduce malpractice risk.
Hospitals using advanced surgical technologies report a 15% reduction in complications and associated malpractice claims. This figure highlights the potential benefits of adopting new medical technologies. However, it’s crucial to balance the advantages of new technologies with the need for proper training and risk management.
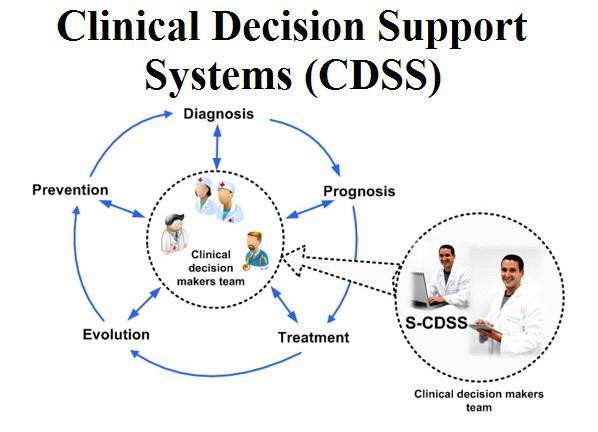
AI and Machine Learning in Healthcare
The use of artificial intelligence and machine learning in medical diagnosis and treatment raises new legal questions about liability when these technologies are involved in medical errors. This emerging field requires careful consideration of ethical and legal implications.
AI-assisted diagnoses have shown a 20% improvement in accuracy for certain conditions. This statistic highlights the potential of AI to enhance medical decision-making. However, it’s important to consider how this improved accuracy might affect the standard of care and liability in cases where AI recommendations are not followed.
35% of healthcare organizations plan to leverage AI for clinical decision support by 2023. This growing adoption of AI in healthcare settings will likely have significant implications for malpractice liability. It raises questions about who is liable when AI-assisted decisions lead to adverse outcomes.
Legal experts predict that AI-related malpractice claims will increase by 30% in the next five years. This projected increase underscores the need for clear guidelines and regulations regarding the use of AI in healthcare. Healthcare providers and institutions must be prepared to navigate these new liability challenges.
Telemedicine Standards of Care
The standard of care in telemedicine practices may differ from traditional in-person medical care. Defining and applying these standards presents unique challenges for healthcare providers and legal professionals alike.
76% of hospitals in the U.S. now use telemedicine services. This widespread adoption of telemedicine has been accelerated by the COVID-19 pandemic. It represents a significant shift in healthcare delivery that requires careful consideration of malpractice liability issues.
Studies show that telemedicine can be as effective as in-person care for 60% of primary care visits. This statistic suggests that telemedicine can be a viable option for many patients. However, it’s crucial to establish clear guidelines for when telemedicine is appropriate and when in-person care is necessary.
Malpractice insurers report a 35% increase in telemedicine-related claims since 2019. This rise in claims highlights the need for specific standards of care for telemedicine practices. Healthcare providers must be aware of the unique challenges and limitations of remote care to minimize malpractice risk.
Specialty-Specific Standards of Care
Different medical specialties may have varying standards of care, which can complicate malpractice cases involving multiple specialists or interdisciplinary care. Understanding these nuances is crucial for healthcare providers and legal professionals.
Subspecialty care accounts for 68% of all malpractice claims. This statistic highlights the complexity of modern healthcare and the importance of specialty-specific standards of care. It underscores the need for clear communication and coordination among specialists to prevent malpractice claims.
Interdisciplinary care teams report 25% fewer malpractice claims than single-specialty practices. This figure suggests that collaborative, team-based approaches to patient care can reduce malpractice risk. It emphasizes the importance of effective communication and coordination among healthcare providers.
Courts consider specialty-specific guidelines in 80% of malpractice cases involving multiple specialties. This trend reflects the recognition that different medical specialties may have distinct standards of care. It underscores the importance of staying current with specialty-specific guidelines and best practices.
Emerging Medical Specialties
Newly emerging medical specialties face unique challenges in establishing their standards of care. This process impacts malpractice litigation in these fields and requires careful consideration from both medical and legal perspectives.
The number of recognized medical specialties has increased by 15% in the past decade. This growth reflects the increasing complexity and specialization of medical knowledge. It also presents challenges in defining standards of care for these new specialties.
Emerging specialties face 40% higher malpractice premiums due to undefined standards of care. This increased cost reflects the uncertainty and risk associated with new medical fields. It underscores the importance of establishing clear guidelines and best practices in emerging specialties.
It takes an average of 5-7 years for a new medical specialty to establish widely accepted care standards. This period of uncertainty can be challenging for healthcare providers in new specialties. It emphasizes the need for ongoing research and professional consensus-building in emerging medical fields.
International Standards and Global Healthcare
International medical standards increasingly influence malpractice cases, especially in our globalized healthcare environment. Understanding these global influences is crucial for healthcare providers operating in international contexts.
20% of malpractice cases now involve some aspect of international medical standards. This statistic reflects the increasingly global nature of healthcare. It highlights the need for healthcare providers to be aware of international best practices and standards.
Hospitals adhering to international accreditation standards report 30% fewer malpractice claims. This figure suggests that adopting globally recognized standards can help reduce malpractice risk. It underscores the potential benefits of aligning local practices with international benchmarks.
Cross-border telemedicine services have increased by 70% since 2019, raising new standard of care questions. This rapid growth in international telemedicine presents unique challenges in defining applicable standards of care and determining jurisdiction in malpractice cases.
The Role of Expert Witnesses in Malpractice Litigation
Expert witnesses play a crucial role in medical malpractice cases, providing specialized knowledge to help courts understand complex medical issues. The selection, preparation, and impact of expert witnesses significantly influence malpractice litigation outcomes.
Expert witness testimony is used in 95% of medical malpractice trials. This statistic underscores the critical role that expert witnesses play in malpractice litigation. Their testimony often forms the foundation for determining whether a healthcare provider met the standard of care.
Courts reject expert testimony in 25% of cases due to lack of qualifications or reliability. This figure highlights the importance of selecting qualified, credible expert witnesses. It also underscores the need for thorough preparation and vetting of expert testimony.
Challenges in Expert Witness Selection
Selecting appropriate expert witnesses involves complex considerations of credentials, experience, and potential biases. This process can significantly impact the outcome of malpractice cases and requires careful attention from legal teams.
40% of malpractice cases involve conflicting expert testimonies. This statistic highlights the often subjective nature of expert opinions in complex medical cases. It underscores the importance of presenting clear, well-supported expert testimony.
Juries are 60% more likely to side with the party presenting the most credentialed expert. This figure emphasizes the importance of selecting highly qualified expert witnesses. It suggests that the credentials and reputation of expert witnesses can significantly influence jury decisions.
30% of expert witnesses in malpractice cases have faced professional misconduct allegations. This statistic raises concerns about the reliability and credibility of some expert witnesses. It underscores the importance of thorough background checks and vetting processes in expert witness selection.
Daubert Standard and Expert Testimony
The Daubert standard affects the admissibility of expert testimony in medical malpractice cases. Understanding this standard is crucial for attorneys and expert witnesses to ensure that testimony meets legal requirements and effectively supports their case.
The Daubert standard is used in 70% of U.S. jurisdictions to evaluate expert testimony. This widespread adoption of the Daubert standard has significant implications for the preparation and presentation of expert testimony in malpractice cases.
Courts exclude expert testimony based on Daubert challenges in 35% of malpractice cases. This stat
Courts exclude expert testimony based on Daubert challenges in 35% of malpractice cases. This statistic highlights the rigorous scrutiny that expert testimony faces under the Daubert standard. It underscores the importance of ensuring that expert opinions are based on reliable scientific methods and principles.
Daubert hearings increase pre-trial costs by an average of 25% in malpractice cases. This additional expense reflects the time and resources required to prepare for and conduct Daubert hearings. It emphasizes the need for thorough preparation and strong scientific foundations for expert testimony.
Peer Review of Expert Testimony
Peer review of expert testimony can improve the quality and reliability of expert evidence in malpractice cases. This process helps ensure that expert opinions align with current medical knowledge and standards.
Peer-reviewed expert testimony is 40% less likely to be challenged in court. This statistic suggests that peer review can enhance the credibility and reliability of expert testimony. It underscores the potential benefits of subjecting expert opinions to scrutiny by other professionals in the field.
Medical societies offering peer review services report a 50% increase in requests since 2015. This trend reflects growing recognition of the value of peer review in enhancing the quality of expert testimony. It suggests an increasing emphasis on ensuring that expert opinions align with current medical consensus.
Courts are 30% more likely to admit expert testimony that has undergone peer review. This figure highlights the legal system’s recognition of the value of peer review. It suggests that peer-reviewed testimony may be viewed as more reliable and credible by judges and juries.
The Impact of Expert Testimony on Jury Decisions
Expert testimony significantly influences jury decisions in medical malpractice trials. Understanding effective strategies for presenting expert evidence is crucial for both plaintiffs and defendants in malpractice cases.
Juries rule in favor of the party with the most persuasive expert testimony in 65% of cases. This statistic underscores the critical role that expert witnesses play in shaping jury decisions. It highlights the importance of not only selecting qualified experts but also ensuring they can effectively communicate complex medical concepts to lay jurors.
Visual aids used by expert witnesses increase jury comprehension by 40%. This figure emphasizes the value of clear, visual presentations in helping juries understand complex medical information. It suggests that effective use of visual aids can significantly enhance the impact of expert testimony.
Juries spend an average of 30% more time discussing expert testimony than other evidence. This statistic highlights the weight that juries give to expert opinions in their deliberations. It underscores the importance of ensuring that expert testimony is clear, compelling, and memorable.
Cross-Examination Strategies for Expert Witnesses
Effective techniques for cross-examining expert witnesses in malpractice cases can challenge or support their testimony. These strategies play a crucial role in shaping the jury’s perception of expert evidence.
Successful cross-examination reduces the impact of opposing expert testimony by up to 50%. This statistic highlights the potential power of effective cross-examination in malpractice cases. It underscores the importance of thorough preparation and skilled questioning techniques.
Attorneys spend an average of 15 hours preparing for each hour of expert witness cross-examination. This figure reflects the complexity and importance of expert witness testimony in malpractice cases. It emphasizes the need for meticulous preparation to effectively challenge or support expert opinions.
35% of expert witnesses admit to changing their opinion under effective cross-examination. This statistic underscores the potential impact of skilled cross-examination on expert testimony. It suggests that well-prepared attorneys can significantly influence the weight given to expert opinions by juries.
Ethical Considerations for Expert Witnesses
Expert witnesses in medical malpractice cases face significant ethical obligations. Potential conflicts of interest can arise, requiring careful navigation to maintain the integrity of the legal process.
25% of expert witnesses report feeling pressured to alter their testimony to favor their client. This statistic raises concerns about the potential for bias in expert testimony. It underscores the importance of ethical guidelines and professional integrity for expert witnesses.
Medical boards have sanctioned 10% of frequent expert witnesses for ethical violations. This figure highlights the potential consequences of ethical breaches in expert testimony. It emphasizes the need for expert witnesses to maintain high ethical standards and professional integrity.
80% of medical societies now offer ethics training for members serving as expert witnesses. This trend reflects growing recognition of the ethical challenges faced by expert witnesses. It suggests an increasing emphasis on ensuring that expert testimony adheres to ethical guidelines and professional standards.
As we conclude this comprehensive exploration of medical malpractice claims, it’s clear that navigating this complex landscape requires expertise and dedication. This is where Ultra Law can make a significant difference. With their specialized knowledge in personal injury law, including medical malpractice, Ultra Law is well-equipped to guide you through the intricacies of your case.
Ultra Law’s commitment to client-centered representation ensures that your unique circumstances are fully understood and addressed. Their team of experienced attorneys stays up-to-date with the latest developments in medical malpractice law, including evolving standards of care and the nuances of expert testimony.
If you’re dealing with the aftermath of a potential medical malpractice incident, don’t hesitate to reach out to Ultra Law. They offer free initial consultations to discuss your case and operate on a contingency fee basis, meaning you don’t pay unless they win your case. This approach ensures that justice is accessible to all, regardless of financial circumstances.
Take the first step towards understanding your rights and options. Contact Ultra Law today to schedule your free consultation and let their expertise work for you in navigating the complexities of medical malpractice claims.
Learnings Recap
- Medical malpractice claims have far-reaching impacts on healthcare providers, patients, and the broader healthcare system.
- Effective communication and patient safety initiatives play crucial roles in preventing malpractice claims.
- The economics of medical malpractice insurance significantly influence healthcare practices and policies.
- Healthcare reforms and evolving standards of care continue to shape the landscape of medical malpractice.
- Expert witnesses play a pivotal role in malpractice litigation, requiring careful selection and preparation.
- Understanding the psychological impact of malpractice claims on healthcare providers is crucial for addressing systemic issues in healthcare delivery.