In 2023, Nevada saw a 5.2% increase in workers’ compensation claims. This uptick reminds me of my first day teaching adults with autism about workplace rights. I was nervous, but their eagerness to learn made it a rewarding experience. Today, we’ll explore the ins and outs of las vegas workers compensation in 2024.
Table of Contents
-
Understanding the Basics of Workers’ Compensation in Las Vegas
-
Navigating the Claims Process
-
Dispute Resolution and Appeals
-
2024 Updates and Considerations
-
Employer Responsibilities and Best Practices
-
Emerging Trends in Workers’ Compensation
Understanding the Basics of Workers’ Compensation in Las Vegas
Workers’ compensation in Las Vegas is a crucial system that protects employees injured or ill due to their job. It’s designed to provide medical benefits and wage replacement while shielding employers from lawsuits. In 2024, grasping this system’s nuances is essential for both employees and employers in Las Vegas.
The Nevada Industrial Insurance Act governs workers’ compensation in the state. It’s not just a set of guidelines; it’s the backbone of workplace safety and employee protection. Employers with one or more employees must carry workers’ compensation insurance. This requirement ensures that even small businesses contribute to the safety net for workers.
Let’s talk numbers for a moment. According to the U.S. Bureau of Labor Statistics, private industry employers in Nevada reported 34,600 nonfatal workplace injuries and illnesses in 2022. This resulted in a total recordable cases (TRC) incidence rate of 3.4 cases per 100 full-time equivalent workers. These stats highlight the ongoing need for robust workers’ compensation systems.

Source: getforesight.com
For a comprehensive understanding of personal injury cases, including those related to workplace accidents, check out our accident guide. It’s a valuable resource that complements the information we’re discussing here.
Eligibility Criteria
Not all workers in Las Vegas automatically qualify for workers’ compensation. It’s crucial to understand who’s eligible to ensure proper claim filing and resolve disputes effectively. Coverage extends to most full-time and part-time employees, including undocumented workers. This inclusive approach reflects the diverse workforce in Las Vegas.
However, independent contractors, domestic workers, and certain agricultural workers may be excluded from coverage. The distinction between employees and independent contractors can be particularly tricky. Eligibility is determined by factors such as employment status and nature of work. It’s not just about job titles; the actual working relationship matters.
Here’s a real-world example: A part-time bartender at a Las Vegas casino who slips and falls during their shift would likely be eligible for workers’ compensation. On the flip hand, a freelance photographer hired for a one-time event at the same casino might not qualify. The key difference? The nature of their employment relationship with the casino.
Covered Employees
Most full-time and part-time employees in Las Vegas are covered by workers’ compensation. This includes undocumented workers, ensuring broad protection for the workforce. It’s a testament to the system’s goal of protecting all workers, regardless of their immigration status.
Coverage typically begins on the first day of employment. There’s no waiting period or probation. This immediate coverage is crucial for new hires who might be unfamiliar with their work environment and potentially more susceptible to injuries.
Volunteers and casual workers may be excluded from coverage in certain situations. It’s not a one-size-fits-all scenario. Some employers may elect to cover otherwise excluded workers voluntarily. This flexibility allows businesses to extend protection to a wider range of individuals contributing to their operations.
|
Employee Type |
Typically Covered? |
|---|---|
|
Full-time |
Yes |
|
Part-time |
Yes |
|
Undocumented |
Yes |
|
Volunteers |
No* |
|
Independent Contractors |
No* |
|
Domestic Workers |
No* |
*May be covered in certain circumstances or if employer elects coverage
Qualifying Injuries and Illnesses
For an injury or illness to be covered by workers’ compensation in Las Vegas, it must be work-related. This includes accidents on the job site, occupational diseases, and repetitive stress injuries. The “arising out of and in the course of employment” standard is used to determine work-relatedness. It’s not always black and white, and each case is evaluated on its merits.
Occupational diseases must meet specific criteria to be compensable. These aren’t your everyday illnesses. They’re conditions that are directly related to the nature of the work performed. For instance, a construction worker developing silicosis from prolonged exposure to silica dust would likely qualify.
In some cases, mental health conditions caused by work may also be eligible for coverage. However, stress-related mental health claims often require a higher burden of proof. It’s a complex area that reflects the growing recognition of mental health in the workplace.
Recent developments have brought mental health more into focus. Workers’ Compensation News reports on new guidelines for rating permanent work-related mental impairments in Nevada, ranging from Category 0 (no impairment) to Category 6 (maximum impairment). This update acknowledges the serious impact mental health issues can have on workers.
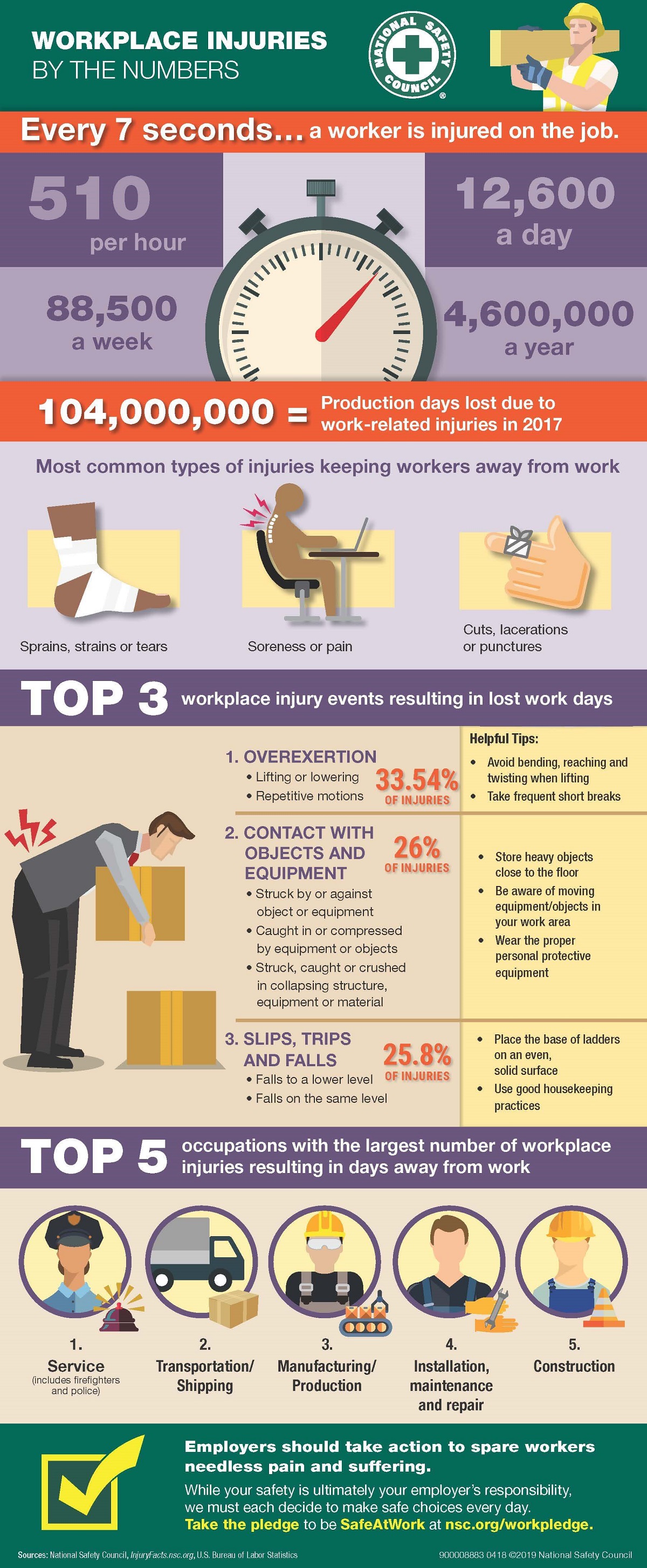
Source: nsc.org
Benefits Available
Las Vegas workers’ compensation offers various benefits to injured workers. Each benefit type is designed to address different aspects of recovery and financial stability, ensuring comprehensive support for those affected by workplace injuries or illnesses. It’s not just about covering medical bills; it’s about holistic support during recovery.
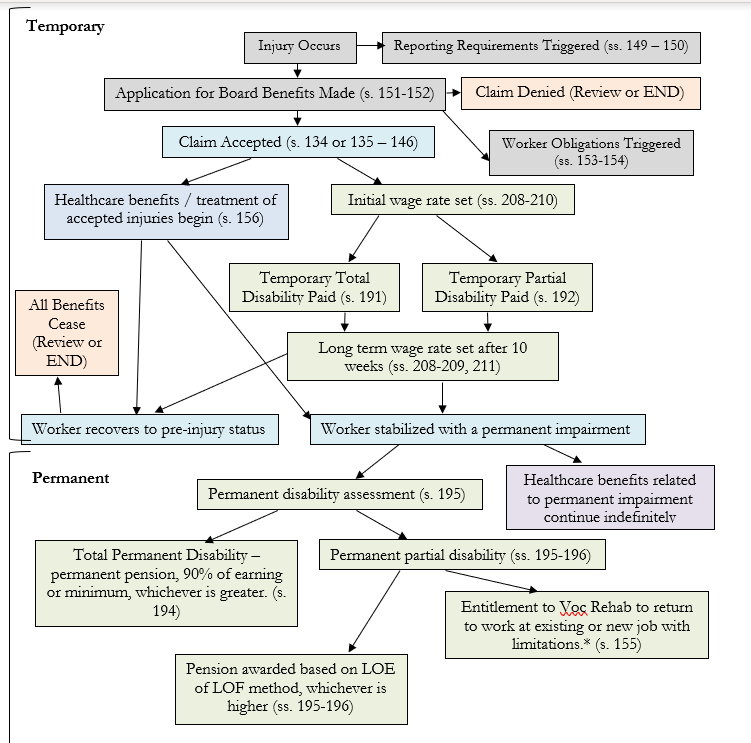
Benefits are categorized into medical, wage replacement, and permanent disability compensation. The type and duration of benefits depend on the severity and nature of the injury. It’s a nuanced system that aims to provide appropriate support for each unique situation.
There are statutory limits on certain benefit amounts and durations. These limits help balance the needs of injured workers with the financial sustainability of the system. It’s a delicate balance, but one that’s crucial for the long-term viability of workers’ compensation in Las Vegas.
Source: youtube.com
Medical Benefits
Workers’ compensation in Las Vegas covers all necessary medical treatment related to the work injury. This includes doctor visits, hospital stays, medications, and rehabilitation services. There’s no deductible or co-pay for these services, ensuring injured workers receive the care they need without financial burden.
Medical benefits are provided without a time or monetary limit if treatment is reasonable and necessary. This open-ended approach ensures that workers with severe or chronic injuries can receive ongoing care as needed. It’s a crucial aspect of the system that supports long-term recovery.
Injured workers have the right to choose their treating physician from an approved list. This choice is significant because the treating physician plays a key role in determining the course of treatment and work status. Preauthorization may be required for certain treatments or procedures, adding a layer of oversight to ensure appropriate care.
Consider a construction worker who suffers a severe back injury on a job site in Las Vegas. Their workers’ compensation would cover all necessary medical treatments, from initial emergency care to long-term physical therapy, without any out-of-pocket expenses for the worker. This comprehensive coverage allows the worker to focus on recovery without financial stress.
Temporary Total Disability (TTD) Benefits
When a worker is completely unable to work during recovery, Temporary Total Disability benefits provide wage replacement. In Las Vegas, these benefits are calculated at 66 2/3% of the worker’s average monthly wage, subject to state-mandated maximums. It’s a significant financial support system for workers during their recovery period.
TTD benefits begin after a 5-day waiting period, which is waived if disability lasts more than 20 days. This waiting period helps manage short-term absences while ensuring substantial support for more serious injuries. The maximum TTD benefit is adjusted annually based on the state’s average weekly wage, ensuring that benefits keep pace with economic changes in Las Vegas.
Benefits continue until the worker reaches maximum medical improvement or returns to work. This duration-based approach ensures support throughout the recovery process, adapting to each worker’s unique situation. In Nevada, the maximum TTD benefit rate for 2024 is set at 66 2/3% of the state’s average weekly wage, reflecting the system’s responsiveness to economic conditions.
Source: keymedia.com
Understanding TTD benefits is crucial for accident victims, as explained in our comprehensive accident guide. It’s an essential resource for navigating the complexities of workplace injuries and compensation.
Permanent Partial Disability (PPD) Benefits
Permanent Partial Disability benefits compensate workers who have permanent impairments but can still work in some capacity. The amount is based on a complex rating system that considers the worker’s age, occupation, and the extent of their impairment. It’s a nuanced approach that aims to provide fair compensation for long-term impacts on earning capacity.
PPD ratings are determined using the AMA Guides to the Evaluation of Permanent Impairment. This standardized approach ensures consistency in evaluations across different cases and medical providers. The rating process involves a medical evaluation by a qualified physician, providing an objective assessment of the worker’s condition.
PPD benefits can be paid in a lump sum or as monthly payments, depending on the rating percentage. This flexibility allows for tailored solutions that best meet the needs of injured workers. The choice between lump sum and monthly payments can have significant financial implications, and workers often benefit from professional advice when making this decision.
Navigating the Claims Process
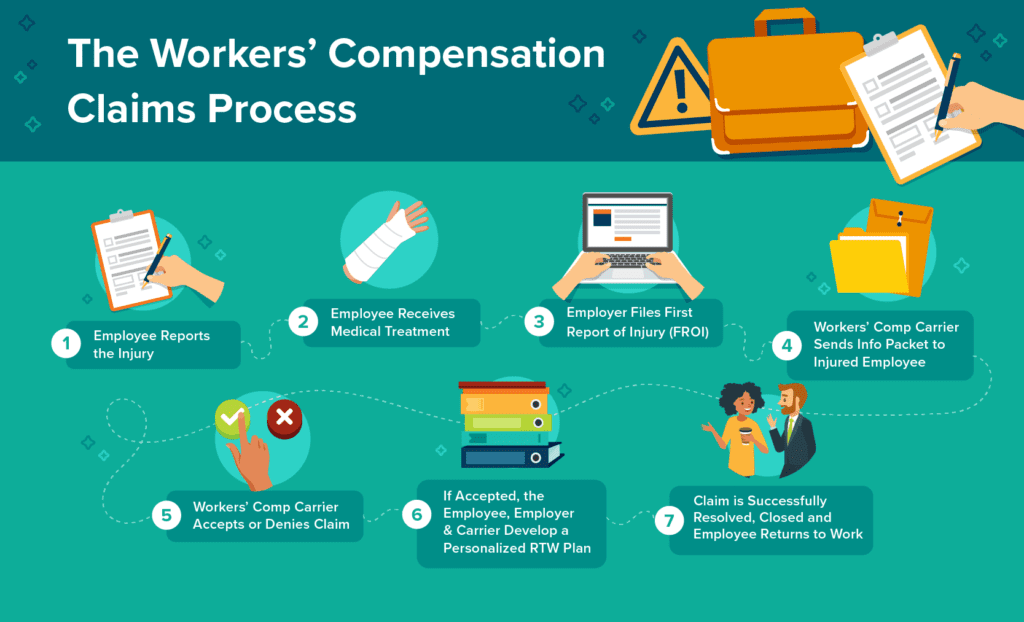
Filing a workers’ compensation claim in Las Vegas involves several steps and deadlines. Understanding this process is crucial for ensuring that injured workers receive their entitled benefits promptly. Both employees and employers have specific responsibilities in this process, and navigating it effectively can make a significant difference in the outcome.
The claims process is governed by strict timelines set by Nevada law. These timelines are not just guidelines; they’re legal requirements that can impact the validity of a claim. Failure to meet deadlines can result in claim denials or penalties, underscoring the importance of prompt action and attention to detail.
Source: ffvamutual.com
Reporting the Injury
Timely reporting is critical in the workers’ compensation claims process. Failing to report within the specified timeframe can jeopardize the worker’s right to benefits. It’s not just a formality; it’s a crucial first step that sets the entire claims process in motion.
Late reporting can lead to claim denials or delays in benefit payments. The reasons for this are twofold: it becomes harder to establish the work-relatedness of the injury as time passes, and it can raise suspicions about the validity of the claim. Prompt reporting helps ensure a smoother, more straightforward claims process.
Employers are required to maintain records of all reported injuries. This documentation is essential for compliance, risk management, and potential future investigations. It’s not just about individual claims; it’s about building a comprehensive picture of workplace safety and injury patterns.
Employee Responsibilities
Workers must notify their employer of the injury in writing within 7 days. This requirement applies to both sudden accidents and gradually developing conditions. For occupational diseases, notice must be given within 7 days of discovering the condition is work-related. It’s crucial to provide detailed information about how, when, and where the injury occurred.
Verbal notification is not sufficient; written notice is required by law. This written requirement serves several purposes: it creates a clear record of the injury report, it ensures that all necessary information is communicated, and it helps prevent misunderstandings or disputes about whether a report was made.
Employees should keep a copy of the injury report for their records. This personal copy can be invaluable if questions or disputes arise later in the claims process. It’s a simple step that can provide significant protection and peace of mind for injured workers.
Failure to report within the 7-day window doesn’t automatically disqualify a claim, but it can complicate the process. Late reporting may require additional evidence or explanation to support the claim, potentially delaying benefits or increasing the risk of denial. The key is to report as soon as possible, even if you’re unsure about the severity of the injury.
For example, if a hotel housekeeper in Las Vegas strains their back while lifting a heavy mattress, they should immediately report the injury to their supervisor in writing, detailing the date, time, and circumstances of the incident, even if they initially think it’s just a minor strain. This prompt reporting protects their rights and initiates the support process.
Employer Responsibilities
Employers must file a C-3 Form (Employer’s Report of Industrial Injury or Occupational Disease) with their insurer within 6 working days of receiving notice of the injury. This form initiates the official claim process and is crucial for timely benefit provision. It’s not just paperwork; it’s the formal start of the workers’ compensation process.
Employers are required to provide employees with a C-1 form (Notice of Injury or Occupational Disease) within 3 working days of the reported injury. This form serves as an official record of the injury report and provides important information to the employee about their rights and responsibilities in the claims process.
Failure to file the C-3 form can result in administrative fines. These penalties are designed to ensure employer compliance and protect workers’ rights to timely claim processing. It’s in everyone’s best interest for employers to meet these filing deadlines promptly and accurately.
Employers must also notify their insurance carrier of any fatalities within 48 hours. This rapid reporting requirement for fatal incidents underscores the seriousness of workplace fatalities and the need for immediate action and investigation. According to the U.S. Bureau of Labor Statistics, fatal work injuries in Nevada totaled 60 in 2022, up from the previous year. Nationwide, a total of 5,486 fatal work injuries were recorded in 2022, a 5.7-percent increase from 5,190 in 2021. These statistics highlight the ongoing importance of workplace safety and proper incident reporting.
Medical Treatment and Evaluations
Proper medical documentation and adherence to treatment protocols are essential for a successful claim. In Las Vegas, the process of obtaining medical treatment and undergoing evaluations is structured to ensure fair and comprehensive care for injured workers. It’s a system designed to balance the needs of workers with the requirements of the workers’ compensation system.
Medical providers must be approved by the Nevada Division of Industrial Relations. This approval process ensures that treating physicians are familiar with workers’ compensation requirements and can provide appropriate care within the system’s guidelines. It’s not just about medical expertise; it’s about understanding the unique context of work-related injuries.
Treatment guidelines are established to ensure consistent and appropriate care. These guidelines help standardize treatment approaches while allowing for individual case variations. They’re not rigid rules but rather evidence-based frameworks to guide medical decision-making. Utilization review processes may be used to evaluate the necessity of certain treatments. This review system helps control costs and ensure that treatments are medically necessary and appropriate for the specific injury. It’s a balancing act between providing comprehensive care and managing resources effectively.
Choosing a Healthcare Provider
In 2024, Las Vegas workers have the right to choose their treating physician from a list of authorized providers, unless their employer has a managed care organization (MCO) in place. This choice is pivotal as the treating physician plays a significant role in determining the course of treatment and work status. The initial choice of physician can be changed once within the first 90 days of treatment. This provision allows workers to switch providers if they’re unsatisfied with their initial choice, ensuring they receive care they’re comfortable with. Subsequent changes require approval from the insurer or a hearing officer, adding a layer of oversight to the process. MCOs may restrict provider choice but must offer a sufficient selection of qualified physicians. While this might seem limiting, it’s designed to ensure that workers receive care from providers experienced in occupational injuries and familiar with the workers’ compensation system.

Source: workers-compensation-doctors.com For more information on selecting the right medical provider after an accident, visit our comprehensive accident guide. It’s a valuable resource for navigating the complexities of medical care in workers’ compensation cases.
Independent Medical Examinations (IMEs)
Insurers may request Independent Medical Examinations to assess the extent of the injury and treatment progress. These evaluations can significantly impact claim decisions and benefit determinations. They’re not routine check-ups; they’re specialized assessments that can shape the course of a claim. IMEs must be conducted by physicians not involved in the worker’s treatment. This requirement ensures an unbiased evaluation, free from any potential influence of the ongoing treatment relationship. It’s about getting a fresh, objective perspective on the worker’s condition. Workers have the right to have their own physician present during an IME. This provision allows for a level of oversight and can help workers feel more comfortable during the examination. It’s a safeguard against potential misunderstandings or misinterpretations of the worker’s condition. IME findings can be contested if the worker disagrees with the results. This right to challenge provides an important check in the system, ensuring that workers aren’t unfairly disadvantaged by a single evaluation. It’s part of the broader system of checks and balances in workers’ compensation.
Dispute Resolution and Appeals
When disagreements arise in workers’ compensation cases, Las Vegas provides a structured process for resolution. This system ensures fair treatment for all parties involved, balancing the needs of workers, employers, and insurers. The Nevada Department of Administration oversees the dispute resolution process. They’re not just bureaucrats; they’re the referees in the complex game of workers’ compensation disputes. Their role is crucial in maintaining the integrity and fairness of the system. There are specific timelines for each stage of the dispute resolution process. These timelines keep cases moving forward, preventing unnecessary delays that could harm injured workers or burden employers. It’s a system designed for efficiency and fairness.
Source: wiki.clicklaw.bc.ca
Informal Resolution Methods
Before escalating to formal hearings, parties are encouraged to resolve disputes through less adversarial means. These methods can lead to quicker resolutions and maintain better relationships between workers, employers, and insurers. It’s about finding common ground without the need for lengthy legal battles. Informal resolution methods are voluntary but strongly encouraged. They’re not mandatory, but they’re often the smartest first step in resolving disagreements. These methods can save time, money, and stress for all involved. Successful informal resolutions can be formalized into binding agreements. This means that even though the process is informal, the outcomes can have real, enforceable weight. It’s a way to get the best of both worlds: flexibility in the process and certainty in the outcome.
Mediation Services
The Nevada Department of Administration offers free mediation services to help resolve disputes between injured workers, employers, and insurers. Mediation provides a neutral forum where all parties can discuss issues and work towards mutually acceptable solutions. It’s not about winning or losing; it’s about finding a middle ground that works for everyone. Mediators are trained professionals with expertise in workers’ compensation law. They’re not just facilitators; they’re knowledgeable guides who can help parties navigate the complexities of their disputes. Their expertise can be invaluable in finding creative solutions to seemingly intractable problems. Mediation sessions are confidential and non-binding. This confidentiality encourages open and honest communication, allowing parties to explore solutions without fear of compromising their positions if the case goes to a formal hearing. The non-binding nature means parties can try mediation without risking their right to pursue other options if it doesn’t work out.
Benefit Review Conferences
These informal meetings allow parties to discuss issues and potentially reach agreements without the need for a formal hearing. Benefit review conferences are facilitated by a neutral party and can address a wide range of disputes related to workers’ compensation claims. They’re like mediation’s cousin, offering another avenue for resolution before things get formal. Conferences are typically scheduled within 30 days of a request. This quick timeline helps keep cases moving and prevents disputes from festering. It’s about addressing issues while they’re still fresh and before positions become entrenched. Parties can bring representatives or attorneys to the conference. While these meetings are informal, having professional representation can help ensure that all aspects of the dispute are properly addressed. It’s about being prepared and informed, even in an informal setting.
Formal Hearings and Appeals
When informal methods fail, the formal hearing process provides a structured approach to resolving disputes. This process involves presenting evidence and arguments before administrative law judges who have the authority to make binding decisions on workers’ compensation matters. It’s the legal equivalent of bringing out the big guns. Formal hearings are conducted under the Nevada Administrative Procedure Act. This act provides a framework for how these hearings should be conducted, ensuring consistency and fairness across different cases. It’s not just about resolving individual disputes; it’s about maintaining the integrity of the entire system. Decisions from formal hearings can be appealed to higher administrative and judicial levels. This multi-tiered appeal system ensures that there are checks and balances in place, allowing for correction of errors and consideration of complex legal issues. It’s a safeguard against injustice, providing multiple opportunities for review.
Hearings Before a Hearing Officer
The first level of formal dispute resolution is a hearing before a hearing officer. Here, evidence is presented and a decision is rendered. It’s like a mini-trial focused specifically on workers’ compensation issues. Hearing officers are appointed by the Department of Administration. They’re not judges in the traditional sense, but they have specialized knowledge in workers’ compensation law. Their expertise allows them to navigate the complexities of these cases efficiently. Parties have the right to be represented by an attorney at the hearing. While not required, legal representation can be crucial in presenting a strong case and navigating the procedural requirements of the hearing. It’s about putting your best foot forward in a formal legal setting.
Appeals to the Appeals Officer
If dissatisfied with the hearing officer’s decision, parties can appeal to an appeals officer within 30 days. This level involves a more comprehensive review of the case, including all evidence and testimony from the initial hearing. It’s a second bite at the apple, a chance to correct any errors or oversights from the first hearing. Appeals officers have the authority to affirm, reverse, or modify the hearing officer’s decision. They’re not just rubber stamps; they conduct a thorough review and can make significant changes to the original decision. Their role is crucial in ensuring the accuracy and fairness of the system. New evidence is generally not allowed at this stage unless there’s good cause. This restriction helps maintain the integrity of the process and encourages parties to present all relevant information at the initial hearing. It’s about fairness and efficiency, preventing endless cycles of new evidence and appeals. A recent Kentucky Supreme Court decision may influence how Las Vegas courts interpret the “course and scope of employment” for traveling employees. The case involved a worker injured while buying souvenirs on a work trip. This ruling could potentially expand the definition of work-related activities, especially for employees who travel as part of their job. It’s a reminder that workers’ compensation law is constantly evolving, influenced by decisions from across the country.
2024 Updates and Considerations
As we move into 2024, several updates and emerging trends are shaping the landscape of workers’ compensation in Las Vegas. These changes reflect technological advancements, evolving workplace risks, and shifts in policy approaches. It’s a dynamic field, constantly adapting to new realities. Legislative changes may impact benefit calculations and coverage definitions. These adjustments often aim to balance the needs of workers with the financial sustainability of the system. Staying informed about these changes is crucial for all stakeholders in the workers’ compensation system. Technological innovations are influencing claim processing and medical care delivery. From AI-powered claim assessments to telemedicine consultations, technology is revolutionizing how workers’ compensation operates. It’s not just about efficiency; it’s about improving outcomes for injured workers.
Technological Advancements in Claims Processing
The integration of AI and machine learning is streamlining the claims process, potentially leading to faster benefit disbursement and more accurate fraud detection. These technological advancements are changing how workers’ compensation claims are handled in Las Vegas. It’s like having a super-smart assistant helping manage claims. AI algorithms are being used to predict claim outcomes and identify high-risk cases. This predictive capability allows for early intervention in potentially complex cases, improving outcomes and reducing costs. It’s about being proactive rather than reactive in claim management. Blockchain technology is being explored for secure and transparent record-keeping. This could revolutionize how claim information is stored and shared, enhancing security and reducing disputes over claim histories. It’s a high-tech solution to age-old problems of data management and transparency.
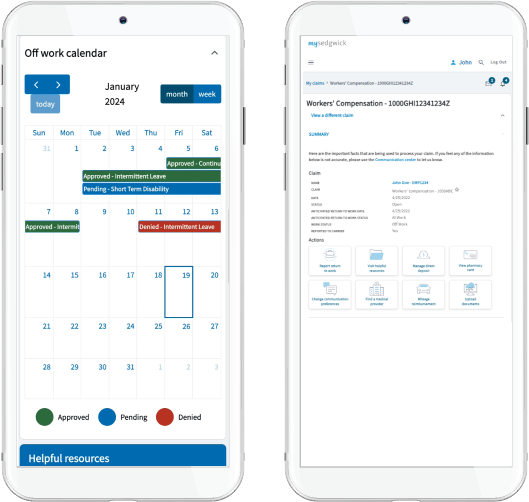
Digital Claim Filing Systems
New user-friendly platforms allow for easier claim submission and tracking, reducing paperwork and expediting the process for injured workers. These digital systems are making it simpler for employees to initiate and monitor their claims, while also improving efficiency for employers and insurers. It’s about bringing workers’ compensation into the digital age. Mobile apps are increasingly used for real-time claim updates and communication. This instant access to information helps keep all parties informed and engaged in the claim process. It’s putting the power of information directly in the hands of workers and employers. Digital systems often integrate with existing HR and payroll software. This integration streamlines the entire process, from injury reporting to benefit calculation. It’s about creating a seamless flow of information across different aspects of employee management.
Source: sedgwick.com
Telemedicine for Work-Related Injuries
The expansion of telemedicine services in workers’ compensation cases provides quicker access to medical consultations, especially beneficial for minor injuries or follow-up appointments. This trend is particularly relevant in Las Vegas, where it can help workers in remote areas access care more easily. It’s bringing medical expertise to workers, wherever they are. Telemedicine visits are typically reimbursed at the same rate as in-person visits. This parity in reimbursement encourages the adoption of telemedicine, ensuring that providers are fairly compensated for their services. It’s about removing financial barriers to this convenient form of care. Virtual physical therapy sessions are becoming more common for certain injuries. These online sessions allow for continuous care and monitoring, even when in-person visits aren’t feasible. It’s expanding the reach and effectiveness of rehabilitation services.
Emerging Workplace Risks and Coverage
As the nature of work evolves, so do the potential risks and corresponding coverage needs in Las Vegas. The workers’ compensation system is adapting to address new types of workplace injuries and illnesses that may not have been common in the past. It’s a constant process of identifying and responding to new challenges. Emerging risks are leading to new categories of compensable injuries. From repetitive stress injuries in office environments to mental health issues exacerbated by work stress, the definition of work-related injuries is expanding. It’s about recognizing the full spectrum of ways work can impact health. Coverage expansions may require adjustments to insurance premiums. As the scope of covered conditions grows, insurers need to recalibrate their risk assessments and pricing models. It’s a delicate balance between comprehensive coverage and financial sustainability.
Remote Work Considerations
With more employees working from home, there’s increased focus on defining work-related injuries in remote settings and adjusting coverage accordingly. This shift presents new challenges in determining compensability and implementing safety measures for home offices. It’s about extending workplace protections beyond traditional office boundaries. Home ergonomic assessments are becoming part of some employers’ safety programs. These assessments help ensure that remote workers have safe and comfortable work setups, reducing the risk of injuries. It’s a proactive approach to preventing work-from-home related health issues. The concept of “course and scope of employment” is being redefined for remote work. This redefinition is crucial for determining when and how injuries sustained at home qualify for workers’ compensation. It’s about adapting legal concepts to new work realities. A Las Vegas-based call center employee who trips over a computer cord while working from home may be eligible for workers’ compensation, provided they can demonstrate the injury occurred during work hours and in the designated home office space. This example illustrates the complexities of applying workers’ compensation principles to remote work scenarios.
Mental Health Coverage Expansion
Growing recognition of work-related mental health issues is leading to expanded coverage for conditions like PTSD and chronic stress in certain professions. This expansion reflects a more holistic understanding of workplace health and safety in Las Vegas. It’s about acknowledging that mental health is just as important as physical health in the workplace. Some mental health claims may require a physical injury component to be compensable. This requirement can be controversial, as it may not fully capture the range of work-related mental health issues. It’s an area of ongoing debate and potential future policy changes. Occupations with high stress or trauma exposure may have specific mental health provisions. This targeted approach recognizes that certain jobs carry inherent psychological risks. It’s about tailoring coverage to the unique challenges of different professions.
|
Mental Health Condition |
Typically Covered? |
Special Requirements |
|---|---|---|
|
PTSD |
Yes* |
Often requires specific triggering event |
|
Chronic Stress |
Sometimes |
May need to demonstrate work-relatedness |
|
Anxiety |
Sometimes |
Often requires physical manifestation |
|
Depression |
Sometimes |
May need to show direct work causation |
*Coverage may vary depending on occupation and circumstances
Legislative Changes and Policy Updates
2024 brings new regulations and policy adjustments that impact workers’ compensation in Las Vegas, requiring stakeholders to stay informed and adapt. These changes aim to improve the system’s effectiveness and fairness for both workers and employers. It’s a continuous process of refinement and improvement. Policy updates often reflect changes in workplace demographics and injury patterns. As the workforce and work environments evolve, so too must the policies governing workers’ compensation. It’s about keeping the system relevant and effective in a changing world. Stakeholder input, including from labor unions and business associations, influences legislative changes. This collaborative approach ensures that changes reflect the needs and concerns of all parties involved in the workers’ compensation system. It’s about finding balanced solutions that work for everyone.
Benefit Rate Adjustments
Annual updates to maximum and minimum benefit rates reflect changes in the state’s average weekly wage, affecting compensation calculations for injured workers. These adjustments ensure that benefits keep pace with economic changes in Las Vegas. It’s a way of maintaining the real value of benefits over time. The maximum TTD rate for 2024 is set at 66 2/3% of the state’s average weekly wage. This standardized approach ensures that benefit caps are consistently aligned with broader economic indicators. It’s about maintaining fairness and adequacy in benefit levels. Minimum compensation rates are also adjusted annually. This ensures that even lower-wage workers receive meaningful benefits if injured on the job. It’s a safeguard against benefits falling below a certain threshold.
Expanded Coverage for Occupational Diseases
Recent legislative efforts have broadened the definition of occupational diseases, potentially including more conditions related to long-term workplace exposures. This expansion recognizes the evolving nature of workplace health risks in Las Vegas. It’s a step towards more comprehensive protection for workers facing diverse health challenges. New occupational diseases may be added based on scientific evidence and industry trends. This dynamic approach allows the system to keep pace with emerging research and changing work environments. It’s about staying responsive to new understandings of work-related health impacts. The burden of proof for occupational disease claims may vary depending on the condition. Some diseases with clear workplace links might have a presumption of work-relatedness, while others may require more extensive documentation. This nuanced approach balances worker protection with the need for evidence-based claims.
Employer Responsibilities and Best Practices
In 2024, Las Vegas employers face evolving responsibilities in managing workers’ compensation, from prevention to claim handling. Implementing effective strategies can lead to safer workplaces, lower insurance costs, and better outcomes for injured workers. It’s about creating a win-win situation for both employers and employees. Employers have legal obligations under both state and federal workplace safety laws. These dual requirements create a comprehensive framework for protecting workers and managing risks. It’s not just about compliance; it’s about fostering a culture of safety and responsibility. Proactive safety measures can result in lower workers’ compensation insurance premiums. This financial incentive aligns business interests with worker protection, encouraging ongoing investment in safety programs. It’s a practical demonstration of how safety and fiscal responsibility can go hand in hand.
Workplace Safety Programs
Robust safety measures reduce injury risks and can lower insurance premiums. Effective programs create a culture of safety, benefiting both employees and the company’s bottom line. It’s about making safety an integral part of daily operations, not just an afterthought. OSHA guidelines form the foundation for many workplace safety programs. These federal standards provide a baseline for safety practices across industries. However, truly effective programs go beyond mere compliance, tailoring approaches to specific workplace needs. Data-driven approaches help identify high-risk areas and tailor prevention strategies. By analyzing incident patterns and near-misses, employers can focus their efforts where they’re most needed. This targeted approach maximizes the impact of safety initiatives.
Safety Training and Education
Regular, updated safety training tailored to specific industry risks is crucial for accident prevention and compliance. It empowers employees to recognize hazards and take appropriate precautions. Effective training turns workers into active participants in maintaining a safe workplace. Training frequency and content should align with job roles and identified risks. A one-size-fits-all approach often falls short; customization is key. This targeted training ensures that workers receive information relevant to their specific tasks and environments. Interactive and scenario-based training often proves more effective than passive methods. Engaging employees in realistic simulations or problem-solving exercises can improve retention and application of safety principles. It’s about making safety training memorable and practical.

Source: knowledgecity.com
Ergonomic Assessments
With an uptick in repetitive stress injuries, employers are encouraged to conduct regular ergonomic evaluations, especially in office and manufacturing settings. These assessments can prevent long-term health issues and boost productivity. It’s an investment in both worker health and operational efficiency. Ergonomic assessments should consider both physical workspace and job task design. This holistic approach addresses not just furniture and equipment, but also work processes and schedules. It’s about creating an environment that supports the body’s natural movements and limitations. Wearable technology is increasingly used to monitor and improve ergonomics. These devices can provide real-time feedback on posture and movement, allowing for immediate corrections. It’s a high-tech solution to age-old problems of workplace strain and injury.
Return-to-Work Programs
Effective return-to-work strategies benefit both employers and employees, facilitating a smoother transition back to the workplace after an injury. These programs can reduce claim costs and improve employee morale. They’re about getting workers back on their feet while supporting the company’s operational needs. Successful programs often involve collaboration between HR, supervisors, and healthcare providers. This team approach ensures that all aspects of the worker’s recovery and job requirements are considered. It’s about creating a supportive network for the returning employee. Return-to-work programs can positively impact experience modification rates for insurance premiums. By reducing the duration and cost of claims, these programs can lead to lower insurance costs over time. It’s a clear example of how investing in employee well-being can yield financial benefits.
Modified Duty Options
Developing a range of modified duty positions allows injured workers to return to work sooner. This approach can reduce overall claim costs and maintain employee engagement during recovery. It’s about finding productive roles that accommodate medical restrictions while contributing to the company’s operations. Modified duty should be meaningful work that contributes to the company’s operations. Assigning busy work or make-work tasks can be demoralizing and counterproductive. The goal is to provide tasks that are valuable to both the worker and the employer. Job banks listing potential modified duty tasks can streamline the accommodation process. This proactive approach allows for quick placement of returning workers in suitable roles. It’s about having a ready arsenal of options to facilitate smooth transitions back to work.
Coordination with Healthcare Providers
Maintaining open communication with treating physicians helps ensure that return-to-work plans align with medical recommendations and restrictions. This coordination is crucial for successful reintegration of injured workers. It’s about creating a bridge between medical care and workplace realities. HIPAA-compliant processes must be in place for sharing medical information. Balancing the need for information with privacy requirements is crucial. It’s about respecting worker confidentiality while obtaining necessary details for effective accommodation. Some employers use nurse case managers to facilitate communication with healthcare providers. These professionals can serve as liaisons, translating medical information into practical workplace accommodations. They’re the interpreters in the complex language of recovery and work capabilities.
Compliance and Record-Keeping
Staying compliant with workers’ compensation regulations requires diligent record-keeping and reporting practices. Proper documentation protects employers and ensures smooth claim processing. It’s the paperwork that underpins the entire system, providing a trail of evidence and accountability. Electronic record-keeping systems can streamline compliance and improve data accessibility. These digital solutions offer advantages in organization, searchability, and data analysis. They’re tools that turn record-keeping from a chore into a strategic asset. Regular internal audits help identify and correct compliance issues proactively. These self-checks can catch and rectify problems before they become serious violations. It’s about maintaining a state of continuous improvement and vigilance.
OSHA Reporting Requirements
Employers must understand and adhere to OSHA reporting timelines for workplace injuries, which may differ from workers’ compensation claim deadlines. Prompt reporting is crucial for compliance and can impact workplace safety initiatives. It’s about meeting legal obligations while contributing to broader safety data collection efforts. Severe injuries must be reported to OSHA within 24 hours, fatalities within 8 hours. These tight timelines underscore the seriousness of significant workplace incidents. They’re designed to enable quick responses and investigations when needed most. OSHA 300 logs must be maintained for all recordable injuries and illnesses. These logs provide a comprehensive picture of workplace safety over time. They’re not just records; they’re tools for identifying trends and areas needing improvement.
Documentation Best Practices
Maintaining detailed records of safety meetings, incident reports, and claim-related communications is crucial for defending against potential disputes or audits. Good documentation practices can also inform future prevention strategies. It’s about creating a robust paper trail that tells the story of workplace safety efforts and incidents. Standardized forms and protocols ensure consistency in documentation across the organization. This uniformity makes it easier to compare incidents, spot patterns, and maintain compliance. It’s about creating a common language for safety documentation throughout the company. Digital document management systems can improve accessibility and searchability of records. These systems transform static documents into dynamic, analyzable data sets. They’re the modern solution to the age-old challenge of managing vast amounts of critical information.
Emerging Trends in Workers’ Compensation
The workers’ compensation landscape in Las Vegas is evolving, with new trends shaping how claims are handled and benefits are delivered. Staying abreast of these trends helps all stakeholders navigate the system more effectively. It’s about anticipating changes and adapting proactively. Technological innovations are driving many of the emerging trends in workers’ compensation. From AI-powered claims processing to telemedicine, technology is reshaping every aspect of the system. It’s a digital revolution in a field traditionally dominated by paperwork and in-person interactions. Changing workforce demographics are influencing policy and practice adaptations. As the nature of work and the composition of the workforce change, so too must the approaches to worker protection and compensation. It’s about ensuring the system remains relevant and effective for all workers.
Alternative Dispute Resolution Methods
There’s a growing emphasis on resolving workers’ compensation disputes through less adversarial means. These approaches can lead to faster resolutions and reduced costs, benefiting both workers and employers. It’s about finding common ground without the need for prolonged legal battles. ADR methods can include mediation, arbitration, and facilitated negotiations. Each of these approaches offers a different path to resolution, allowing for flexibility in addressing diverse types of disputes. They’re tools in the toolkit of conflict resolution, each suited to different situations. Some jurisdictions are piloting mandatory ADR programs for certain types of disputes. These initiatives aim to streamline the resolution process and reduce the burden on formal hearing systems. They’re experiments in finding more efficient ways to address disagreements.
Online Dispute Resolution Platforms
Digital platforms facilitating virtual mediations and negotiations are becoming more prevalent. They offer convenience and efficiency in dispute resolution, particularly valuable in a post-pandemic world. These platforms are breaking down geographical barriers and speeding up the resolution process. AI-powered platforms can help identify common ground and suggest resolution options. By analyzing patterns in successful resolutions, these systems can offer insights that might not be immediately apparent to human mediators. They’re like having a super-smart assistant in the negotiation room. Virtual platforms often include features for document sharing and real-time collaboration. These tools recreate the dynamics of in-person meetings in a digital space. They’re about making remote negotiations as effective and interactive as face-to-face sessions.
Early Intervention Programs
Proactive approaches to addressing potential disputes early in the claims process are gaining traction. These programs aim to prevent escalation to formal hearings, saving time and resources for all parties involved. It’s about nipping problems in the bud before they bloom into full-blown disputes. Early intervention often involves specialized claims adjusters or ombudsmen. These professionals are trained to identify and address issues that could lead to disputes. They’re the peacekeepers of the workers’ compensation world, working to maintain harmony in the claims process. Data analytics are used to flag claims with high dispute potential for early intervention. By analyzing patterns in historical claims data, these systems can predict which current claims are most likely to result in disagreements. It’s about using the power of data to prevent conflicts before they start.
Holistic Approach to Worker Recovery
The focus is shifting towards comprehensive recovery strategies that address not just physical injuries but overall worker well-being. This approach recognizes the interconnected nature of physical, mental, and social health in recovery. It’s about treating the whole person, not just the injury. Biopsychosocial models of care are becoming more common in workers’ compensation treatment plans. These models consider psychological and social factors alongside physical symptoms. They’re about understanding recovery as a complex process influenced by multiple factors. Outcome measures are expanding to include quality of life and functional capacity indicators. It’s no longer just about physical healing; it’s about restoring the worker’s ability to engage fully in work and life. These broader measures provide a more complete picture of recovery success.
Biopsychosocial Model of Care
Treatment plans increasingly consider psychological and social factors alongside physical symptoms. This model recognizes their impact on recovery and return to work, leading to more personalized and effective care strategies. It’s about understanding that healing is more than just physical repair. Psychological screening tools are being incorporated into initial injury assessments. These tools help identify mental health concerns that could impact recovery. They’re about catching and addressing psychological barriers to healing early in the process. Social factors such as family support and job satisfaction are considered in treatment planning. These elements can significantly influence a worker’s motivation and ability to recover. They’re the often-overlooked aspects of healing that can make a big difference in outcomes.
Wellness Programs Integration
Some employers are integrating workers’ compensation with broader wellness initiatives. This approach aims to improve overall employee health and reduce injury risks, creating a more holistic view of workplace health and safety. It’s about seeing worker well-being as a continuum, not just a response to injuries. Integrated programs may include fitness incentives, nutrition counseling, and stress management. These components work together to create a healthier, more resilient workforce. They’re about preventing injuries by promoting overall health and well-being. Data from wellness programs can inform targeted injury prevention strategies. By understanding the health profiles and risk factors of their workforce, employers can tailor their safety initiatives more effectively. It’s about using comprehensive health data to create smarter, more focused prevention efforts. For more information on how wellness programs can prevent workplace accidents, visit our accident guide. It offers insights into creating comprehensive health and safety strategies that benefit both workers and employers.
Learnings Recap
-
Workers’ compensation in Las Vegas is a complex system requiring careful navigation by both employees and employers.
-
Timely reporting and adherence to claim processes are crucial for ensuring proper benefits and care.
-
Emerging trends like telemedicine and holistic recovery approaches are reshaping the workers’ compensation landscape.
-
Employers play a vital role in creating safe workplaces and facilitating effective return-to-work programs.
-
Staying informed about legislative updates and leveraging technology can improve outcomes for all stakeholders.
-
Alternative dispute resolution methods are gaining prominence, offering faster and less adversarial solutions.




